Bariatric surgery complications:
- Are almost never life-threatening (99.9% survival rate)
- Are non-existent for about 93% of patients (30-day complication rate is 7%)
- Risk can be further minimized in a number of ways
- Differ depending on which procedure you choose
Read the sections below for everything you need to know about weight loss surgery complications.
TABLE OF CONTENTS
Click on any of the topics below to jump directly to that section
- Obesity Risks Vs Surgery Risks
- How to Reduce Risk
- Complications By Procedure
- List & Definitions
- Patient Community & Expert Advice
SECTION SUMMARY:
- Remaining obese is much more dangerous than having bariatric surgery
- Obesity is the 2nd leading cause cause of premature death (after smoking)
- There are almost too many life-shortening obesity health problems to list. Issues such diabetes and heart disease are two of the most dangerous
- Bariatric Surgery has 99.9% survival rate and 7% of patients have complications
Comparing the risk of remaining obese to the risk of bariatric surgery is like comparing apples to oranges:
- Obesity risks are stretched out over a long period of time. Problems can take many years to develop and worsen. Ultimately, having obesity leads to a decreasing quality of life, increasing severity of many health issues, and an increasing risk of premature death.
- Bariatric surgery risks tend to fall within the first 30 days after surgery. For the more involved procedures that lead to the most weight loss, the mortality (death) rate is about 0.1% or 1 out of every 1,000 patients. However, 7% of these patients experience complications related to surgery. The less involved procedures have much less weight loss and a much lower risk of complications.
The simplest way to think about it: If you choose to have a more involved bariatric surgery (gastric sleeve, gastric bypass, Lap-Band, or duodenal switch), you are willing to go through surgery for the benefit of:
- Losing between 50% and 90+% of your excess weight
- Curing or dramatically improving all of your obesity-related health problems
- Dramatically reducing your risk of premature death
- Eliminating obesity discrimination issues
- Improving self-confidence and self esteem
The extent to which you experience each of these benefits depends on:
- Which procedure you choose
- How closely you adhere to diet and lifestyle guidelines set by your surgeon
If you choose a less-involved procedure (gastric balloon or AspireAssist), you reduce your risk of dying to almost 0%. The trade-off is much less weight loss (20 to 30% of excess weight) and much less noticeable improvement in your health.
See our Bariatric Surgery Risks page for more information.
SECTION SUMMARY:
- Educate yourself
- Educate your family & friends
- Lose weight before your surgery
- Address your health problems before your surgery
- Choose an experienced surgeon
- Get tested for sleep apnea syndrome before your surgery
- Exercise ASAP after your surgery
- Use standard methods to prevent deep vein thrombosis (see below)
- Follow your surgeon’s advice closely
- Put a good support system in place and use it
About 7% of bariatric surgery patients undergoing a high-weight-loss procedure (gastric sleeve, gastric bypass, Lap-Band, or duodenal switch) will experience complications (2).
Reduce your risk of complications by (click each to learn more):
1. Educate yourself
You will be better prepared to make the right decisions if you know exactly what to expect before, during, and after surgery.
Start on one of the following pages depending on how much you already know:
- If you’re not sure if having a weight loss procedure is right for you:
- If you know it’s right for you, but you don’t know which procedure to have:
- If you’ve narrowed down the procedures, but you still can’t decide,review in detail the patient guides for your chosen procedures:
- If you know all about each procedure, but you need to know more about insurance and out-of-pocket costs, review our:
- Insurance Guide (if you have insurance)
- Cost Guide (if you don’t have insurance)
- If you’re ready to talk with a surgeon about one or two procedures, but you’re not 100% sure about what to expect after surgery:
2. Educate family & friends
Family and friends are often the deciding factor for whether you stay on track. For example, if your spouse or partner is snacking and eating junk food, you will be tempted to do the same.
To avoid issues like this, educate your closest family members and friends before you have surgery by:
- Asking them to read the same resources listed in the Educate Yourself section above
- Allowing them to be a part of the decision making process when selecting a procedure
- Asking them to come with you to your surgeon office visits
- Having them attend a patient support group with you after surgery
3. Lose weight before surgery
The higher your body mass index (BMI), the more likely you are to have bariatric surgery complications.
Most bariatric surgeons will not require you to lose weight before surgery, but some surgeons and insurance companies may require you to have a physician-observed bariatric diet and weight loss surgery exercise program before they approve your procedure.
4. Address health problems before surgery
Obesity-related health problems prior to surgery are directly correlated with developing complications in the first 180 days following surgery (3). Talk with your surgeon about how to reduce your risk if you have any of the following conditions:
- Sleep apnea and gastroesophageal reflux disease (GERD) are the prbe-operative conditions that result in the highest risk for bariatric surgery complications.
- If you have had deep vein blood clots (blood clots in legs or arms), a pulmonary embolism or blood clotting problems in the past, you have a higher risk of experiencing them following bariatric surgery.
- High blood pressure prior to surgery can increase your risk of blood clotting problems after surgery.
- Diabetes, sleep apnea and arthritis can determine your risk for sepsis.
Test Your Risk Level
If you want more details about your personal risk level, talk with your surgeon about one of the following tests:
- Metabolic Acuity Score (MAS) – Rates your risk on a scale of 1 to 4 and, according to the researchers, “can help reduce post-surgical complications by 65% and hospital readmission rates by more than 80%” (4).
- Obesity Surgery Mortality Risk Score (OS-MRS) – Measures patients’ risk of being one of the less than 0.2% who die from surgery complications within 30 days following the procedure (5).
- M-SCORE VTE Risk Prediction – Uses a series of risk factors to help surgeons choose the best procedure based on patient risk level and to identify risk factors that can be reduced prior to surgery (6).
5. Choose an experienced surgeon
Working with a more experienced surgeon significantly reduces your risk of complications. For example:
- One study (over 15,000 patients) found these differences depending on how many procedures a surgeon performed over a 3-year period (7):
- Fewer than 100 procedures: 4% complication rate
- More than 250 procedures: 2% complication rate
- Another study (over 14,700 patients) found these 30-day complication rate differences (8) based on the number of procedures performed by the surgeon and their
hospital:
- Fewer than 50 procedures at low-volume (under 125 procedures) hospitals: 0.98% complication rate
- More than 50 procedures at high-volume (300+ procedures) hospitals: 0.30% complication rate
6. Get tested for sleep apnea syndrome before surgery
Sleep apnea significantly increases both surgical and post-surgical risks. This is an easy problem to avoid since it can be diagnosed and treated well in advance of surgery.
Unfortunately, according to a UC Davis School of Medicine study of over 1,300 prospective patients, as high as 25% of prospective patients have undiagnosed sleep apnea prior to surgery (9).
Talk with your surgeon about conducting a sleep study to find out if you have sleep apnea.
7. Use standard methods to prevent deep vein thrombosis
Deep vein thrombosis (DVT) is a risk after any surgery, bariatric or otherwise. It happens when a blood clot forms inside a deep vein (such as those found in the leg or pelvis).
DVT can be life-threatening if the blood clot comes loose then travels to and blocks the the arteries in your lungs. It is especially concerning for patients with a history of blood clotting problems.
Your surgeon should talk with you about standard preventive measures, including:
- Blood thinners
- Compression stockings
8. Exercise as soon as possible after surgery
The quicker you can get up and moving after surgery, the lower your risk of complications.
Start as soon as possible after surgery by:
- Sitting up
- Hanging legs off the bed
- Breathing exercises
- Leg exercises
- Start walking as soon as your surgeon allows it
Be aggressive, but don’t overdo it.
See the following pages for more information:
9. Follow surgeon’s advice
Many patients start to stray from their surgeon’s advice shortly after returning home. Unsurprisingly, weight-loss surgery patients who stick to a schedule of 3, 6, and 12-month follow-up visits with their doctors see greater improvements or remission of their diabetes, high blood pressure, and high cholesterol than patients who skip their visits (10).
Don’t let yourself slip. Maintain contact with your surgeon and dietitian, and follow their advice to the letter to avoid complications and side effects and to maximize weight loss and health improvements after surgery.
10. Have & use a good support system
It is nearly impossible to succeed without the support of those close to you, and your chance of long-term success increases greatly if you’re able to talk with others who understand and will listen without passing judgement.
Successful patients have the following support, at a minimum:
- Supportive family and friends who help you avoid temptation and tell you when you start to slip
- A good weight loss surgery support group that you attend regularly
Other helpful support resources include:
- Online weight loss surgery forums and blogs
- Books written by weight loss surgery patients
See our Weight Loss Surgery Support section for more information.
SECTION SUMMARY:
- Read about the possible complications of gastric sleeve, gastric bypass, the Lap-Band, Duodenal Switch, AspireAssist, & the gastric balloon below
Complications and side effects are more common and more pronounced among the more-involved, higher-weight-loss procedures:
- Gastric sleeve
- Gastric bypass
- Lap-Band
- Duodenal switch
They can be especially pronounced for the two procedures that rearrange your digestive system (they also lead to the most long-term weight loss):
- Gastric bypass
- Duodenal switch
Complications and side effects are less common and less pronounced among the less-involved, lower-weight-loss procedures:
- Gastric balloon
- AspireAssist
To simplify: the more weight loss a procedure results in, the higher the risk of complications and side effects.
Tap here to expand list of complications by procedure.
| Issue | Gastric Sleeve | Gastric Bypass | Gastric Balloon | Lap-Band | Duodenal Switch | AspireAssist |
|---|---|---|---|---|---|---|
| Abscess | – | – | ||||
| Band Problems (band erosion, band infection, band intolerance, band leak, band slippage) | – | – | – | – | ||
| Blood Clots | – | – | ||||
| Bowel Obstruction | – | – | ||||
| Deep Vein Thrombosis | – | – | ||||
| Evisceration & Incisional Hernia | – | – | ||||
| Gastric Fistula | – | – | ||||
| Gastrointestinal Leaks | – | – | – | |||
| General Anesthesia Complications | – | – | ||||
| Heart Attack | – | – | ||||
| Hemorrhage (Bleeding) | – | – | ||||
| Hiatal Hernia | – | – | ||||
| Hypoglycemia | – | – | – | – | – | |
| Infection | – | |||||
| Organ Injury During Surgery | – | |||||
| Peritonitis | – | – | – | |||
| Pneumonia | ||||||
| Port Problems (port flip/inversion or dislodgement, port leak, port infection, port dislocation) | – | – | ||||
| Port Problems (port flip/inversion or dislodgement, port leak, port infection, port dislocation) | – | – | – | – | – | |
| Pouch Dilation | – | – | – | – | – | |
| Pulmonary Embolism | – | – | ||||
| Respiratory Failure | – | – | ||||
| Stenosis/Stricture | – | – | – | |||
| Stoma Obstruction | – | – | – | |||
| Stroke | – | – | ||||
| Thrombophlebitis | – | – | ||||
| Wound Reopening | – | – | ||||
| Wound Sepsis | – | – |
Tap here to expand list of side effects by procedure.
| Issue | Gastric Sleeve | Gastric Bypass | Gastric Balloon | Lap-Band | Duodenal Switch | AspireAssist |
|---|---|---|---|---|---|---|
| Abdominal Discomfort | – | – | – | – | – | |
| Anemia | – | – | – | |||
| Body Aches | – | – | ||||
| Body Feeling Changes | – | |||||
| Bowel Function Changes (diarrhea, constipation, foul-smelling bowel movements and flatulence, difficulty swallowing, gurgling noises) | — | |||||
| Dehydration | – | – | ||||
| Dental Problems | – | – | – | – | – | |
| Dumping Syndrome | – | – | – | – | – | |
| Dyspepsia (Indigestion) | – | – | ||||
| Esophageal Dilation | – | – | ||||
| Esophagitis | – | – | ||||
| Food Trapping | – | – | – | – | – | |
| Gallstones | – | – | ||||
| Gastritis | – | – | ||||
| Gastroesophageal Reflux Disease (GERD) | – | – | ||||
| Hair Loss | – | – | ||||
| Intolerance to Certain Foods | – | |||||
| Kidney Stones | – | – | – | – | ||
| Marginal Ulcers | – | |||||
| Nausea, Vomiting and/or Stomach Cramps | ||||||
| Skin Changes (e.g. acne, dry skin, sagging skin, etc.) | – | – | ||||
| Thrush (Yeast Infection) | – | – | ||||
| Vitamin & Mineral Deficiency / Malnutrition / Malabsorption | – | – | ||||
| Weight Regain | – |
For more information about complications and side effects by weight loss procedure, click the links below:
SECTION SUMMARY:
- A to Z list of complications and definitions
Click on a letter below to jump to a bariatric surgery complication beginning with that letter or scroll down the page to review the complete list of complications, definitions (10), and treatments:
| A | B | C | D | E | F | G | H | I | J | K | L | M | N | O | P | Q | R | S | T | U | V | WXYZ |
Abdominal hernias – a protrusion of an organ or part through connective tissue or through a wall of the cavity in which it is normally enclosed – also called a “rupture”. Most hernias are treated with surgery unless another condition makes surgery inadvisable.
Abscesses – a localized collection of pus surrounded by inflamed tissue. Abscesses are drained percutaneously (through the skin) or through surgery.
Aches – see Body Aches.
Alcohol Use Disorder (AUD) – a physical and emotional dependence on alcohol that leads to the inability to cease drinking, even after serious lifestyle, health, or legal issues.
Anastomotic Leaks happen when the surgical connection made during bariatric surgery leaks digestive contents into the abdomen. See Gastrointestinal Leaks for more.
Anesthesia complications – See General Anesthesia Complications.
Anemia – a condition in which the blood is deficient in red blood cells, in hemoglobin or in total volume. Anemia is a common issue stemming from vitamin deficiency after malabsorptive bariatric surgery procedures.
Anemia following bariatric surgery is routinely treated with iron orally and, when indicated, with intravenous iron infusions; blood transfusions are rarely required. Finding and treating anemia before surgery with iron and ESA therapy has been found to be effective at both avoiding transfusions and reducing surgery risks (11).
- Band Erosion (also called “Band Migration “) – occurs in gastric banding (lap band surgery) and vertical banded gastroplasty patients as these are the only bariatric procedures involving a band. Band erosion occurs when the band actually grows into the stomach. The only treatment is a permanent removal of the band. See our Lap Band Erosion page for more information.
- Band Intolerance– when patients do not respond well (i.e. excessive and continued vomiting) to the band placed during vertical banded gastroplasty or gastric banding (lap band) surgery. Will probably require that the band be permanently removed.
- Band leak (1.1% – 4.9% of lap band patients) – patients can usually tell if their lap band system has a leak if their feelings of restriction (how much they can eat) decrease over time without the doctor unfilling the port. To determine if you have a lap band leak, your doctor may inject colored fluid and take an X-Ray to see if any of the colored fluid is present (from a leak) outside of the lap band system. Surgery is usually required to repair it.
- Band Migration – See Band Erosion.
- Band Slippage – occurs when the lower part of the stomach “slips” up through the band, creating a bigger pouch above the band (only occurs after gastric lap band surgery and vertical banded gastroplasty as these are the only bariatric procedures involving a band). As many as 1 in 10 patients experience this with gastric banding (lap band surgery), and either removing fluid from the lap band or surgery is required to repair it. Symptoms include vomiting and reflux. It is diagnosed by drinking a dye and using X-Ray to observe it. For information about surgical techniques to reduce the risk of slippage, see our Gastric Lap Band Procedure page.
Bleeding – See Hemorrhage.
Blood Clots (also called “thrombus”) – overweight people have a higher risk of developing blood clots during and after any kind of surgery. Blood thinners are usually administered during and after surgery to avoid them, along with special devices that squeeze the lower legs to keep the blood flowing. Walking around periodically after surgery is also very effective. Symptoms of blood clots include swelling or pain in the legs and can be diagnosed by your doctor with an ultrasound. If clots occur, they are treated by a taking a prescribed blood thinner. If left untreated, clots can lead to a pulmonary embolism. Prior to surgery, be sure to tell your doctor whether you or anyone in your family has a history of clotting. Smoking will increase your risk, so if you are a smoker it is recommended that you stop smoking as soon as possible before surgery – no later than two months out. For more information, see our Blood Clot Symptoms, Treatments & Prevention page.
Body Aches – should pass with time. If they become unbearable, talk with your doctor about which pain relievers are safe. You should typically avoid NSAIDs (non-steroidal anti-inflammatory drugs) such as ibuprofen or Aleve.
- Feeling cold – this is caused by both your changed metabolism and weight loss and the fact that you have less fat insulating your body.
- Weak or tired feeling – should pass with time, especially once your new bariatric diet is in place and, as soon as you are feeling up to it, your weight loss surgery exercise program has begun.
Bowel Function Changes (especially more frequent bowel movements and/or foul-smelling flatulence) – bowel function after bariatric surgery may change in a number of ways, (12) including…
- Diarrhea or loose stools (especially after gastric sleeve surgery, duodenal switch, gastric bypass surgery, and mini gastric bypass surgery) – usually completely dependent on diet – you will need to figure out and avoid foods that “trigger ” diarrhea. Could also be the result of lactose intolerance which would require dairy products to be removed from your bariatric diet.
- Constipation (especially after gastric banding (lap band surgery), gastric bypass, mini gastric bypass, and rarely after duodenal switch) – usually fixed by increasing the amount of water you are drinking and taking fiber supplements such as Fiber-Stat’s liquid fiber supplement.
- Foul-smelling bowel movements & flatulence (especially after duodenal switch) – as with diarrhea, it is usually dependent upon diet.
- Difficulty swallowing (“dysphagia”) (after all restrictive procedures) – caused by eating too quickly, too much or not chewing food enough and can usually be fixed by avoiding these issues. (See our Bariatric Eating page to learn about proper eating techniques that will avoid problems.)
- Gurgling Noises – not necessarily uncomfortable or dangerous, but it’s worth noting. Gurgling noises are completely normal and are due to air in the stomach and the different way that your new digestive system pushes the air through. The best way to avoid gurgling noises is to avoid swallowing air (i.e. avoid carbonated beverages, sipping through a straw, eating or drinking too quickly and chewing gum).
Bowel Obstruction – also called an “internal hernia”, is a lifelong risk following bariatric surgery that occurs when the intestines twist and prevent the flow of food and digestive fluids. Patients with this condition usually experience abdominal pain, abdominal swelling, or vomiting. A doctor will confirm the diagnosis with a CAT scan or through surgery, and surgery may or may not be needed to treat it.
Bowel obstructions post-surgery are more commonly associated with adhesions and not internal hernias, although both are known to be associated with post-op bowel obstructions.
Bowel Perforation – See Organ Injury During Surgery.
Cold feeling – See Body Feeling Changes.
Candy Cane Syndrome – A possible complication after gastric bypass, candy cane syndrome happens when a no-longer-functioning part of the small intestine near the new junction of the stomach and small intestine begins to cause abdominal pain, nausea, and vomiting. The “Candy Cane” (the non-functioning portion of the intestine) will need to be laparoscopically removed, but once the “candy cane” is gone, 94% of patients experience complete resolution of their symptoms (REF).
Death – the bariatric surgery mortality rate is extremely low at about 0.135% and has continued to drop over time (13). For a boiled down list of issues that directly contribute to mortality risk, see our Bariatric Surgery Risks page.
Deep vein thrombosis (DVT) is a risk after any surgery (bariatric or otherwise) marked by the formation of a thrombus within a deep vein (as of the leg or pelvis) that may be asymptomatic or accompanied by symptoms (such as swelling and pain). DVT is potentially life-threatening if dislodgement of the thrombus results in pulmonary embolism. Preventive measures are extremely important, especially for those with a history of blood clotting problems. Blood thinners and compression stockings help to reduce the risks. Also see Blood Clots.
Dehydration – an abnormal depletion of body fluids. You will need to drink a significant amount of water in the months following surgery – as much as 2 liters per day. Not doing so can lead to nausea and vomiting which can cause even worse dehydration and other problems. In severe cases of dehydration patients must return to the hospital for IV fluids and vitamins.
Dyspepsia (also called indigestion) – inability to digest or difficulty in digesting food; incomplete or imperfect digestion of food; a case or attack of indigestion marked especially by a burning sensation or discomfort in the upper abdomen. Treatment is usually as simple as changing your diet, such as avoiding greasy foods or only drinking liquids for a certain period of time. Alcohol, aspirin, and other drugs are also causes. If diet changes don’t work, antacids and H2 blockers are sometimes prescribed.
Dysphagia (difficulty swallowing) – See Bowel Function Changes.
Dumping syndrome – we have an entire page dedicated to this topic, but in general it’s a condition characterized by weakness, dizziness, flushing and warmth, nausea and palpitation immediately or shortly after eating. It is produced by abnormally rapid emptying of the stomach especially in individuals who have had part of the stomach removed. See our Dumping Syndrome page for more.
Embolism – See Pulmonary Embolism.
Esophagitis -occurring in less than 1% of patients, esophagitis is the inflammation of the esophagus. It is usually treated non-surgically by making the patient comfortable through a change in diet (avoiding fats and chocolate) and/or avoiding/prescribing certain drugs.
Esophageal dilation – is the enlarging of the esophagus (the opening,not necessarily inflammation) and is usually the result of a restrictive procedure. Most cases can be handled through deflation of the band under radiological control (14). GERDsymptoms and vomiting are more frequent in patients who develop esophageal dilation (15).
Evisceration & Incisional hernia – occur when an internal organ or body part protrudes through a surgical incision. More likely to occur with open procedures than with laparoscopic procedures and usually occurs months after surgery. These are typically repaired with surgery.
Fistulas – see Gastric Fistula.
Food trapping – when food gets caught in one of the small openings in your digestive system. Seen in 1 to 2% of lap band patients and treated by deflating the band entirely until the food passes through (16) (17).
Gallstones – small stones of cholesterol formed in the gall bladder or bile passages. Gallstones can be created following rapid weight loss which leads to their development in as many as 1/3 of bariatric surgery patients. As a result, your surgeon may remove your gallbladder during surgery or prescribe bile salt supplements after surgery.
Gastric fistula – occurring in up to 4% of bariatric surgery patients, a gastric fistula is an abnormal passage that leads from an abscess or hollow organ or part to the body surface or from one hollow organ or part to another (18). Sepsis can follow, and surgery is usually required to fix it.
Gastric fistulas are associated with the stomach (i.e. ‘gastric’). However, not all fistulas are associated with the stomach, and other types can occur (such as from an intestine to intestine anastomosis.)
Related risk/complication of gastric fistula: Wound Sepsis
Gastritis – inflammation, especially of the mucous membrane of the stomach. Symptoms include bloating, excessive belching, a burning sensation in the stomach, loss of appetite, nausea, and vomiting. Eating better may get rid of the problem, or your doctor may prescribe antacids or other over the counter medications.
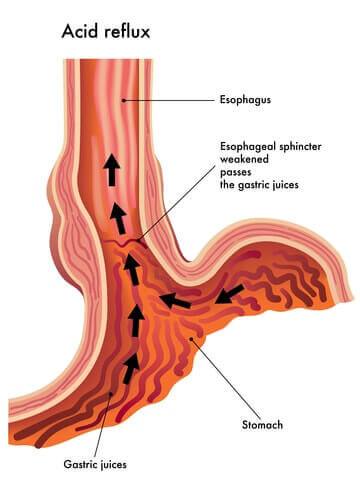
Gastroesophageal reflux disease (GERD) – a highly variable chronic condition that is characterized by periodic episodes of gastroesophageal reflux and usually accompanied by heartburn. It may result in histopathologic changes (change in the microscopic structure) in the esophagus. It also often leads to esophagitis. GERD increases the risk of some bariatric surgery complications such as dumping syndrome and sepsis, but the condition is also improved for many following bariatric surgery (19) (20). Several at-home treatments are effective, including avoiding certain foods and drinks (alcohol, citrus juice, tomato-based food, and chocolate), waiting 3 hours before lying down after a meal, eating smaller meals and elevating your head 8 inches when you lay down. If these don’t work, your doctor may recommend/prescribe antacids, H2 blockers or even Proton Pump Inhibitors (PPI). See our Gastroesophageal Reflux Disease Symptoms and Treatments page (coming soon) for more details.
Gastrointestinal leaks (including staple line leaks) occur when sealed or sutured (stitched) openings leak digestive contents into the abdomen. This can cause infection and abscess. Gastrointestinal leaks occur in as many as 5% of patients and can be repaired as long as it is caught early. Symptoms include fever, severe pain and a high heart rate. In order to prevent leaks, your surgeon should check the surgical connections a number of different ways, including 1) blowing air into the connection and observing whether any gets through and 2) using a dye to check for a leak. Leaks not discovered right away are usually treated by resting the stomach (being fed through an IV), but sometimes surgery is required to fix them.
General anesthesia complications – anesthesia risks increase withage and body mass index (BMI). Other health issues can also increase your risk, including circulatory or respiratory problems. However, anesthesia complications are usually minor and are relatively easy for your doctors to handle.
Hair loss – this can be an alarming side effect of rapid weight loss, but it is only temporary. It happens in about half of all patients in the year following surgery. Proper nutrition is the best defense, including protein and the right bariatric vitamins. Several other treatments can also help, including the application of special shampoos and oils (i.e. Nioxin shampoo, flax seed oil, biotin tablets or powder).
Heart attack (also called myocardial infarction) – an acute episode of heart disease marked by the death or damage of heart muscle due to insufficient blood supply, usually as a result of a coronary thrombosis or a coronary occlusion. Heart attacks are especially characterized by chest pain. The chances of having a heart attack during surgery are less than 0.5% (21).
Hemorrhage (bleeding) – a copious discharge of blood from the blood vessels. One study showed that out of 1,700 laparoscopic bariatric surgery patients only 3 had hemorrhagic complications, none of which needed to be converted to open operations or needed reoperations (22). However, other studies have shown internal bleeding to be as high as 4% following Roux-en-Y gastric bypass surgery. After the surgeon determines the type and severity of internal bleeding, it can be resolved in a number of ways: on its own, replenishing bodily fluids, stopping the use of all anticoagulation drugs and (rarely) by transfusion or reoperation (23).
Hernia – See Evisceration.
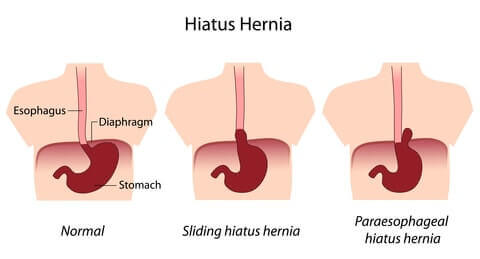
Hiatal Hernia – a hernia in which an anatomical part (such as the stomach) protrudes through the esophageal hiatus of the diaphragm. Hiatal hernias can occur after restrictive procedures when food causes the smaller stomach to bulge and push through the diaphragm. It is also not uncommon for an obese patient to already have a hiatal hernia before surgery. While it can be a “contraindication” for surgery(reason that you may not be able to have the surgery), hiatal hernias can also be repaired during bariatric surgery (24).
Hypoglycemia – Low blood sugar related to excessive insulin production. As a bariatric surgery complication, hypoglycemia is often the result of excessive dumping following Roux-en-Y gastric bypass surgery (25) (26). Medications can usually help mild to moderate conditions, however surgical removal of part or all of the pancreas (which produces insulin) may be required for more serious cases. Symptoms following surgery include rapid heart rate, shaking, sweating, confusion, feeling lightheaded, bad headaches or feeling overly hungry.
Incision(al) hernia – See Evisceration.
Indigestion – See Dyspepsia.
Infection – to contaminate with a disease-producing substance or agent (such as bacteria). Much more common in open surgeries than in laparoscopic surgeries due to the size of the external incisions. Usually treated with antibiotics.
Intolerance to certain foods – With a changed stomach size or digestive system, there will be certain foods that you’ll need to avoid and certain diet habits you’ll need to maintain. See our Bariatric Diet section for more. Also see Bowel Function Changes.
(none)
Kidney stones – stones in the kidney related to decreased urine volume or increased excretion of stone-forming components such as calcium, oxalate, urate, cystine, xanthine and phosphate. The stones form in the urine collecting area (the pelvis) of the kidney and may range in size from tiny to staghorn stones the size of the renal pelvis itself (27). Although additional research is needed, one study suggested that the risk of developing kidney stones increases after bariatric surgery due to changes in digestion and the resulting changes in the chemical makeup of patients’ urine. Click here to learn more.
Leaks – See Gastrointestinal Leak.
Malnutrition/Malabsorption – See Vitamin Deficiency.
Marginal Ulcers – Marginal ulcers are relatively common after Roux-en-Y gastric bypass, mini gastric bypass, and duodenal switch (Scopinaro procedure), and are the most common in the newly created stomach pouch after Roux-en-Y gastric bypass surgery.
Ulcers can usually be avoided by an appropriate bariatric diet , by not smoking and by staying away from NSAIDs (non-steroidal anti inflammatory drugs, including ibuprofen, Aleve, etc.). You can often tell if you have one because of a burning pain in the stomach. Your doctor can confirm ulcers with an endoscopy (a scope than is inserted through your mouth and down your esophagus) and usually treat them with antacids.
Nausea and vomiting are one of the most common side effects of bariatric surgery and are experienced in up to 70% of patients. In one study, patients reported feeling nauseous 1.4 times per week on average after gastric banding (lap band surgery) and 2.6 times per week after gastric bypass surgery (28). They also reported vomiting 0.9 times per week on average with the band and 0.2 times per week after gastric bypass. Following the doctor’s orders regarding your bariatric diet will typically fix or improve the problem. While in the hospital, receiving a larger amount of IV fluids at a faster rate may make you less likely to feel nauseous or vomit (29).
Organ injury during surgery – Caused by surgeon error during surgery. Injuries to your internal organs during surgery are a possibility, especially the bowel, stomach, spleen or esophagus due to their close proximity to the stomach/intestines.
Peritonitis – inflammation of the peritoneum (the smooth transparent serous membrane that lines the cavity of the abdomen, is folded inward over the abdominal and pelvic viscera, and consists of an outer layer closely adherent to the walls of the abdomen and an inner layer that folds to invest the viscera). Peritonitis after bariatric surgery is a serious complication that isusually caused by a gastrointestinal leak. Surgery is required to fixit (30).
Pneumonia – a disease of the lungs that is characterized especially by inflammation and consolidation of lung tissue followed by resolution. It is accompanied by fever, chills, cough, and difficulty breathing, and is caused chiefly by infection. Obese patients are more likely to develop pneumonia post-surgery, so it is important that patients begin deep breathing and coughing exercises following surgery to prevent it. These exercises are much easier after laparoscopic surgery than after open surgery. Should pneumonia develop, it can be treated with antibiotics.
Port problems occur in 20.5% or 1 in 5 gastric banding (lap band) patients (31).Port problems include…
- Port flip/inversion or dislodgement (10.3% of patients) – occurs when the lap band port (where fluids are taken out or added to the band) “flips over”. This is typically not a serious problem and a quick surgical procedure can turn it back over.
- Port Leak (1.1% – 4.9% of patients) – as with a band leak, patients can usually tell if their lap band system has a leak if their feelings of restriction decreases (i.e. the amount they can eat increases) over time without the doctor unfilling the port. To determine if you have a port leak, your doctor may inject colored fluid and take an X-Ray to see if any of the colored fluid is present (from a leak) outside of the lap band system. Surgery is usually required to repair it.
- Port or band infection (1.5% – 5.3% of patients) – if port or band infection occurs, it is usually healed with antibiotics, but removal of the band or port may be necessary.
- Port dislocation (6.9% of patients) – similar to a port flip, a port dislocation means that your port has moved from its original location. It can be fixed with a simple operation under local anesthesia.
Postoperative bleeding – refers to internal bleeding following bariatric surgery.See Hemmorhage.
Pouch dilation – refers to the enlarging of the pouch created after certain types of surgery. For lap band surgery patients, it may be fixed by removing fluid from the band. For all procedures with a pouch, surgery is sometimes required to tighten it (32).
Pulmonary embolism – embolism (the sudden obstruction of a blood vessel by an abnormal particle, such as a bubble, circulating in the blood) of a pulmonary artery or one of its branches that is produced by foreign matter (most often a blood clot originating in a vein of the leg or pelvis) that is marked by labored breathing, chest pain, fainting, rapid heart rate, cyanosis, shock, and sometimes death. Also see Blood Clots and Deep Vein Thrombosis.
(none)
Respiratory failure is a rare but serious complication (33).It occurs when oxygen and carbon dioxide levels fall too far outside of their normal ranges. Hospital treatment includes drugs and ventilation, among other techniques.
Sepsis – See Wound Sepsis.
Skin Changes such as acne or dry skin occur with some patients. The right bariatric diet and bariatric vitamins are your best defense. There are also many over the counter creams and lotions that can help. Worst case, partner with your dermatologist to find a treatment that works.
Spleen damage – See Organ Injury During Surgery.
Staple line leak – See Gastrointestinal Leak.
Stoma obstruction – a partial or complete blockage of the new or altered digestive opening created during bariatric surgery. See Food Trapping.
Stenosis/Stricture – a narrowing or constriction of the diameter of a bodily passage or orifice. This is most common in procedures that rearrange your digestive system such as gastric bypass surgery (up to 8% of patients) and duodenal switch surgery and results from a build-up of scar tissue between your intestine and your reduced stomach or at an intestine-to-intestine connection (anastomosis).
The primary symptom is almost always vomiting, and it is usually treated by inserting and inflating a balloon to stretch the connection between the stomach and intestine. GERD and older age increase the risk of strictures (34).
Stroke– sudden diminution or loss of consciousness, sensation and voluntary motion caused by rupture or obstruction (as by a blood clot )of a blood vessel of the brain. Obese patients have a higher general risk of stroke, and bariatric surgery has been shown to reduce the risk (35).
Thrombus – See Blood Clots
Thrombophlebitis – inflammation of a vein with formation of a thrombus (a clot of blood formed within a blood vessel and remaining attached to its place of origin). The body’s response could be to produce more clots which increase the risk of Deep Vein Thrombosis and Pulmonary Embolism. Also see Blood Clots.
Tired feeling – See Body Feeling Changes.
Thrush (yeast infection) – this can be a side effect of the antibiotics you are on to prevent infection immediately following surgery. Symptoms include changes to your tongue such as a white coating, redness or inflammation. This is easily cured with medicine, so let your doctor know if this starts to develop.
Ulcers – See Marginal Ulcers.
Vitamin and mineral deficiency / malnutrition / malabsorption – symptoms include fatigue, anemia, and osteoporosis and are usually completely avoided by strictly following your doctor’s prescribed vitamin and supplement regimen. You should also have blood work at least semi-annually to make sure that you continue to receive the proper amounts. (See our Bariatric Vitamins page for the problems associated with vitamin deficiency)
Vomiting –See Nausea and Vomiting.
Weak feeling – See Body Feeling Changes.
Weight regain – Most bariatric surgery patients will experience some weight regain after the lowest weight level is reached. See our Weight Gain after Bariatric Surgery page for more.
Wound infection – See Infection.
Wound reopening refers to the opening of the external incisions made during bariatric surgery. It is much more likely to occur following an open procedure than with a laparoscopic procedure.
Wound sepsis (and sepsis in general) – a systemic response typically to a serious localized infection (as of the abdomen or lungs) especially of bacterial origin that is usually marked by abnormal body temperature and white blood cell count, tachycardia and tachypnea; specifically: a systemic inflammatory response syndrome induced by a documented infection.
While wound sepsis can occur from any source of infection, this serious complication often results from a gastric fistula. Due to the risk of wound sepsis following a gastric fistula, the fistula must be treated immediately and effectively in order to avoid sepsis (36). If sepsis does develop, patients are often treated in the intensive care unit with IV fluids and antibiotics.
Yeast infection – See Thrush.
SECTION SUMMARY:
- You can read about the experiences of other gastric sleeve patients
- You Can "Ask the Expert"
Please share the bariatric surgery complications you experienced or are concerned about. Your experiences will help other patients make decisions and avoid pitfalls.
Include anything related to bariatric surgery risks, complications or side effects, such as…
- Which procedure did you have/are you considering?
- Which problems did you experience/are you concerned about?
- Which did your doctor say you were at risk for? How did that compare to what actually happened?
- What did you do/are you doing to minimize your risk?
- How have you addressed the problems?
Questions From Other Visitors*
Click below to see contributions from other visitors to this page.
I had my surgery on December 29, 2010. Six months after my surgery I started smoking occasionally. I smoke about 1 pack of cigarettes every 3 or 4 days. What…
Hair growth problems 10 years after duodenal switch surgery*I had the laparoscopic duodenal switch surgery 10 years ago. Surgically everything has been fine. As we all do, I had problems with thinning hair in the beginning. It grew…
Continuous Belching After Gastric Sleeve Surgery*I am a 62 year old female medical practitioner. I had a gastric sleeve in Sydney, Australia in 2011. I have lost 31 kg (about 70lbs). BMI has decreased from…
Acid Reflux After Gastric Sleeve Surgery*I had gastric sleeve surgery 16 months ago. I have had good weight loss success although my weight loss has stopped. I did lose all of the expected or projected…
Weight Loss, More Energetic But Weak Urination After Sleeve Gastrectomy Surgery*I had my procedure done May 2014, I weighed 230 (only 5' 3" tall) and had high blood pressure. The first 2 weeks prior to surgery I lost 17 pounds.…
Pain Around Lap Band Port*I am a 56 year old female had Lap-Band surgery in 2008. Before surgery, my top weight was 247 lbs. After surgery, my lowest weight was 151 lbs. I've had…
Lost 275 Lbs in 7 Months After Gastric Bypass But Have No Energy & Feel Sick Daily*I had gastric bypass in September of 2014. I started off at 425 pounds, I am now at 275. I am very proud of the weight I have lost. I…
Worried About Complications & Recovery After Gastric Sleeve*I am considering having the Gastic Sleeve surgery in a month's time and am worried about avoiding complications and giving myself enough time to heal before traveling. I've already scheduled…
Loud Stomach Growling After Gastric Bypass*I had the gastric bypass done in 2004. Within the past 2 years I noticed that I can hear my stomach emptying (loud growling / gurgling) and my food moving…
Risk of Leaks After Gastric Sleeve*After you have the gastric sleeve, how long is there a risk of leaking? Do leaks happen frequently after the sleeve? What can the surgeon do to minimize the risk?…
Sugar Causes Vomiting for 3.5 Year Gastric Sleeve Patient*I had a gastric sleeve surgery in April 2011 and have been experiencing frequent vomiting spells (1x week) usually after eating sugar. I had some episodes early on due to…
Rapid Refill of Lap Band After Draining*I had lap band surgery five years ago and lost almost 100 pounds. I had been seeing different Doctors for a depression issue and unfortunately they just kept prescribing medication…
Food Sticking for Lap Band Patient*I had the band fitted 5 years ago and have only lost 4 kilos as a result of the band. Because I was working on mine sites, the surgeon did…
Stomach Pain 3 Months After Gastric Sleeve Surgery*I had the gastric sleeve surgery about 3 months ago. Before surgery I had GERD really bad and was taking prilosec daily. Since the surgery, I have had nothing but…
Roux-en-Y Gastric Bypass Blockage*I had Roux-en-Y gastric bypass in October 2008, and I haven't really followed my doctors advice in the last year or so. My question is, 1 yr ago I had…
Could These Be Side Effects from Lap Band Surgery?*My wife is coming up on a year having her band filled. In the last couple of months she has started being extremely cold all the time, has bruising on…
Questions About Switching from Lap Band to Sleeve*Three years ago I had a lap band put in and did relatively well. I had back surgery and gained almost 100 lbs during the ordeal. I had never been…
My Gastric Band Tube Detached from My Band: Am I In Danger?*I had my band fitted March 2011 in Kent, I received excellent care during the procedure and following the procedure the surgeon arranged for me to have my aftercare in…
Gastric Bypass After Gastric Sleeve: Complications*In September of 2012 I had Gastric Sleeve Surgery but dealt with severe Acid Reflux. My Bariatric Surgeon did two Endoscopies to see if the opening needed to be unblocked…
Acid Reflux & Dry Scratchy Throat Years After Lap Band Surgery*I had lap band surgery several years ago and recently have been experiencing acid reflux and now a dry scratchy and slightly sore throat. I have been taking Nexium which…
Can Gastric Bypass Cause Chronic Bad Breath?*I am considering gastric bypass but I have a friend who had the surgery two years ago and is at goal weight. I have noticed his breath smells bad some…
New Gurgling Sound in Throat & Stomach for Lap Band Patient*My throat and stomach now gurgle with everything I eat or drink. Is this a problem? I have not had a lap band fill in over a year and a…
Wife Losing Too Much Weight & Can't Keep Food Down Since Gastric Sleeve Surgery*My wife had bariatric surgery (vertical sleeve) last March, and now she cant keep anything down. Food, water it doesn't matter. The doctors have given her different meds to try…
Heartburn for the First Time 27 Years After VBG (Vertical Banded Gastroplasty)*It's been 27 years since my VBG (Vertical Banded Gastroplasty). For the first time, within the last 2-3 weeks I've experienced a burning/uncomfortable 'sore throat'. It doesn't matter what I…
After Gastric Bypass I Feel Like I Have a Hair Ball in My Throat*I had gastric bypass 1 month ago and now I feel like I have a hairball or cotton in my throat. Why is that? Other than that, I am doing…
Can my liver be bruised from gastric sleeve surgery?*I was sleeved on Apr. 23rd. It was done laparoscopically. I had elevated liver enzymes prior to the procedure was was given the ok for surgery. The first few days…
Is converting the gastric sleeve to the gastric bypass an effective solution to chronic gastritis and GERD?*My name is Liz and I am 3 months post-op of the gastric sleeve surgery. I decided to have the gastric sleeve surgery after being recommended for it by my…
Soft Stools 2 Years After Roux en Y Gastric Bypass*I had the Roux en Y gastric bypass done about 2 years ago. Since then my stool has changed. It is always very soft I also get diarrhea a lot.…
Long-Term Solution After Failed Lap Band*I underwent a lap band procedure 2 and a half years ago. I lost only 7 kg and regained the weight back. Now I have knee problems and back problems…
Slipped Band - How Do You Know?*I am worried that I have a slipped band, but how can I know for sure? I had lap band surgery in January 2010 and have had really bad reflux…
Help me STOP losing too much weight after DS surgery!*I had BPD/DS surgery in 2004. At the time of surgery I weighed 380 lbs, and I have lost a total of 222 lbs (so far). My problem/concern is what…
Cord from port to lap band entangled her bowel*My Mum had lap band surgery in 2006. She had no weight loss success with it. She had to have the band removed after the plastic tubing from the port…
Feeling of Something Twisting Inside After Gastric Bypass Surgery*I'm wondering if the feeling of something twisting inside is related to my gastric bypass surgery... From time to time I feel a pain just under the bottom of my…
Dilated esophagus and achalasia after lap band surgery*I was recently hospitalized for aspiration pneumonia. They thought it was related to the lap band, so they took it out. The GI doctor did and EGD and said I…
Stabbing pain to the side of my port 3 weeks after lap band surgery*I had my band fitted 3 weeks ago. I have been doing great until Thursday, when I developed a stabbing pain to the side of my port when I move…
Morning sickness syndrome after weight loss surgery*The doctor said that morning sickness syndrome after weight loss surgery was very rare, but I have been in the hospital twice with it and am still suffering from the…
Heartburn and acid reflux after lap band surgery with no weight loss*I had the lap band surgery in 2005, and I haven't lost much weight. I have heartburn after drinking water and acid reflux so bad at night I can't sleep.…
Gastric Sleeve Surgery After Failed Lap Band Surgery*I had lap band surgery which worked great... I lost over 100 pounds (45 kg). But my band slipped (probably my over-stuffing) and it stopped working.I then had a 2nd…
Gurgling sounds in upper chest after gastric sleeve surgery*I had the gastric sleeve, and I notice that I have a gurgling in my upper chest. When I take a bite of pudding it hurts, and I noticed tonight…
Lap band erosion 18 months after surgery*Approx 18 month after my lap band operation I started to experience stomach pain and went for check up at the hospital. It was then found out the band cut…
All fluid in my lap band is gone*I have had the gastric band for five years. Today I went to the hospital to have a fill done to my band and the doctor (who was also x-raying…
RNY Gastric Bypass After Lap Band Surgery*I was banded March 2011. I have to admit I am disappointed in my choice. It is uncomfortable all over - I have problems swallowing and never am full. I…
Side Effects of the Gastric Band (Part Three of Three) - But it's not so bad...*Here I am again with the last of my three articles on the downside of having a gastric band (click here to go back to part one). Of course it's…
Lap band flipped or moved after fill*What happens if your band flips or moves after you had a fill & you feel ill? Originally I was scheduled for gastric bypass. I lost 52 pounds in preparation…
Can you lose so much weight that the port becomes too long?*I have lost 180 pounds since my band surgery 5 yrs ago. My port is sticking out about an inch right under my rib cage. It is VERY uncomfortable. I…
Lap band patient vomiting blood and stomach pain*My wife has had the lap band since approx. 2008. She has been in the hospital (2010) once for an ulcer and severe acid reflux (band way too tight). The…
Sometimes unable to keep down liquids after lap band surgery*I very often go days without being able to drink without it giving me pressure in my chest followed by me having to vomit. I have had my band adjusted…
Lap band surgery complications*Now three years after lap band surgery, I just had 3cc of fluid removed from my band today because I am considering removing the band. Now I taste a back…
Lack of energy after gastric bypass surgery*I had gastric bypass surgery, and now I sometimes lack energy. Do you have any suggestions for this? How about electrolyte supplementation? Thanks for your help!
Post surgical "problems" Vertical Sleeve Gastrectomy/VSG*Bariatric Surgery is not something to been taken lightly. If you're not worried about complications, then you are certainly in a small, small minority. One of the reasons that I…
Is there a chance the REALIZE Band will be recalled because of complication rate?*I had the Realize band which has a higher rate of irritating the stomach - when mine is adjusted enough to work it irritates until it swells my esophagus shut.…
Nicotine Test Before Weight Loss Surgery*I am scheduled to have gastric bypass weight loss surgery in mid-September. When I went for my consultation my doctor said that she was going to do a nicotine test…
Food stays in my throat and espohagus after lap band surgery*Instead of my food moving down quickly it seems to take forever... it moves down a bit then back up a bit and then down and up many times in…
Band Slips w/ the Lap Band*I have had my lap band for over 3 yrs now . The day I hit my goal weight I slipped my band. You slip your lap band a few…
Marginal Ulcers After Gastric Bypass*I have always considered myself one of those gastric bypass success stories. Weight loss was achieved with only a few minor issues. I was a huge proponent of the RNYGB.…
Stricture Plus Hosptial-Acquired Bacteria After Gastric Bypass Surgery*I had gastric bypass surgery Sept. 2007. At first, everything seemed fine. After one week, I could not keep anything down and went back to the hospital. Come to find…
Severe Side Pain, Diarrhea and Hard Stomach 7 Years After Lap Band Surgery*I had the lap band for about 7 years, I only lost 50 pounds and I threw up all the time. In April 2012 I had emergency surgery due to…
Gastric Sleeve Complications: Leak, Stenosis and Kink in Sleeve*June 25, 2012 I underwent 5 1/2 hour surgery for a sleeve gastrectomy. The length of the surgery was due to extreme amount of scar tissue due to a previous…
Acid Reflux After Bariatric Surgery Turned Out to Be Hernia/Twisted Intestines*What I thought was acid reflux was actually an inverted hernia/twisted small intestine. Here's the story... A year after bariatric surgery I was experiencing stabbing pains in what I thought…
Dumping Syndrome with the Gastric Sleeve*Dumping syndrome is something that is usually associated with the RnY gastric bypass procedure. But did you know that you can dump even if you haven't had any sort of…
Weight Loss Surgery Medical Publications: Some things you can't Google*Innovations in the medical world take a while to percolate through to the common woman/man, even if they are being broadcast with screaming headlines by the yellow press. If you…
Side Effects of the Gastric Band (Part Two of Three) - What happens later on as you settle into the band*This is the second of three articles about the less starry-eyed side of having a gastric band. It's a wonderful tool, but you should not be blind to the ifs…
Side effects of having a Gastric Band (Part One of Three): There's good news and bad news*In my family one of the most heated discussions, repeated on a regular basis, was whether pessimism and realism were the same thing. Don't be so pessimistic! was invariably countered…
Research Your Bariatric Surgeon First!*First, this post is NOT against lap band surgery in general. Even though my banded experience was quite traumatic, I still don't regret it. Just wish I had made a…
Secondary-Progressive Multiple Sclerosis (SPMS) & Bariatric Surgery*Hello I'm a 39 year old female with secondary-progressive multiple sclerosis (SPMS) and mild hypertension. I always had issues with weight like most people looking for these types of surgery.…
Collapsing Feeling in Lower Left Side During Difficult Bowel Movements*I'm simply not sure if this is normal but it never happened before my gastric sleeve surgery. I went from lap band to sleeve a little over a year ago.…
Food & Water Won't Stay Down After Bariatric Surgery*I ended up back in the hospital a month after surgery because even water would not stay down. After some tests were run I found out that it was because…
Headache Immediately After Eating - Caused By Weight Loss Surgery?*I had weight loss surgery 11 months ago. Over the past 2 months I have been getting severe sudden headaches immediately after eating. Does this have anything to do with…
Small Bowel Obstruction, Illeus, Bleeding Ulcers, Chronic Anemia, Scar Adhesions*I am a 48-year-old female who underwent Roux-en-Y Gastric ByPass surgery in 2005. On the date of surgery I weighed in at 243 pounds and I l lost my first…
RYGB Surgery for duodenal stenosis*I had quite a few complications, and this was my first ever surgery! I was in a lot of pain post-surgically, mainly in a knot about 1-2cm under my breastbone…
Two RNYs and further complications...*I had a full RNY bypass in 2002. Lost 100 lbs, surgeon left area without references for aftercare. Gained it all back plus more. Had a revision RNY in 2006,…



