Lap-Band surgery (also called adjustable gastric band surgery, or AGB) wraps an adjustable band around the upper part of your stomach. This creates a small stomach pouch above the band that fills up quicker while you’re eating.
As a result, if you are a successful patient:
- You will feel full sooner when you eat, so you eat less
- You will lose between 25% and 75% of your excess weight (e.g., if you’re 100 lbs. overweight, you will lose between 25 and 75 lbs.)
- You will improve or cure your obesity-related health problems and feel better
Read below for everything you need to know about Lap-Band surgery.
TABLE OF CONTENTS
Click on any of the topics below to jump directly to that section
- Before & After Pictures
- How It Works
- Weight Loss
- Health Benefits
- How to Qualify
- Insurance
- Cost Without Insurance
- Preparing for Surgery
- Recovery
- Diet & Life After
- Risks & Downsides
- How Does It Compare to Other Weight Loss Procedures?
- Summary: 7 Steps to Long-Term Weight Loss
- Find a Weight Loss Surgeon
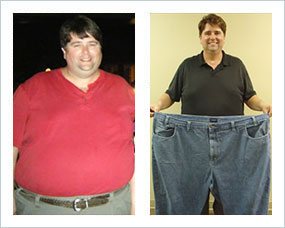
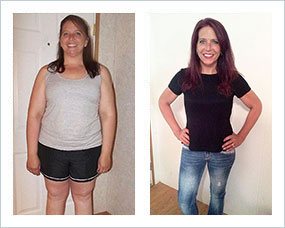
Lap-Band Surgery Before & After Pictures
Before and after weight loss success
Individual results may vary
How Lap-Band Surgery Works
SECTION SUMMARY:
- An adjustable band is wrapped around top portion of your stomach
- A smaller stomach ‘section’ above the band fills up quicker after eating
- You feel full sooner while eating and eat less as a result
The LAP-BAND® procedure is done laparoscopically in one to two hours.
During your procedure, the surgeon will wrap an inflatable band around the upper-middle part of your stomach – think of the inner tube of a bicycle tire. The band connects to a tube that leads to a round half-dollar-sized port just below the skin.
The band, which can be tightened or loosened, creates a smaller stomach “section” above the band which fills up quicker after eating, causing you to feel full sooner while eating and eat less.
As time goes on, your band can be filled and unfilled through a port just below the skin. Filling or “unfilling” makes the band tighter or looser to adjust how full you feel while eating.
Weight Loss After Lap-Band Surgery
SECTION SUMMARY:
- You can lose up to 55% of excess weight within 2 years
- For example, if you’re 5’ 4” and weigh 220 lbs, you will lose up to 42 lbs within 2 years
- If you’re 5′ 9” and weigh 300 lbs, you will lose up to 73 lbs within 2 years
Weight loss happens fast after LAP-BAND® surgery:
- Month 3 Average: About 20% of your excess weight is gone
- Month 6 Average: About 30% of your excess weight is gone
- Month 12 Average: About 40% of your excess weight is gone
- 2 Year Average: More than half of your excess weight is gone
But these are averages. LAP-BAND® surgery patients’ weight loss ranges from 25% to 80% of their excess weight.
Most LAP-BAND® patients reach a weight loss plateau around the 2 year mark.
Click Here to See How Much Weight You Could LoseSee our Lap Band Results page for additional details.
References: (4) (5) (6) (7) (8) (9) (10) (11) (12)
Health Benefits of Lap-Band Surgery
SECTION SUMMARY:
- You can cure or improve your diabetes, sleep apnea, hypertension, and at least 12 other conditions
LAP-BAND® surgery patients experience significant improvement in or a complete “cure” of obesity-related health problems, including those listed in the table below.
Note that patients who have a strict follow-up schedule with their surgeon at 3-, 6-, and 12-months post-op see greater improvements in or remission of their diabetes, high blood pressure (hypertension), and high cholesterol than patients who skip these visits (13).
LAP-BAND® weight loss improves joint health. For every pound of weight lost, there is a 4 pound reduction in pressure on the knee (14). This improves mobility and reduces pain in the knees.
88,000 participants were involved in data collection on cancer research. Results state that patients who undergo weight loss surgery have 33% less risk of developing cancer (15).
Risk rates were even further reduced for obesity-related cancers, including (16):
- Colon cancer
- Postmenopausal breast cancer
- Endometrial cancer
- Pancreatic cancer
Most LAP-BAND® patients experience significant improvement in or a complete “cure” of obesity-related health problems.
Click Here to See A Full List of Health BenefitsHow to Qualify for Lap-Band Surgery
SECTION SUMMARY:
- 30+ body mass index (BMI) required
- If your BMI is under 40, you must have at least one obesity-related health problem
You could be a good candidate for LAP-BAND® surgery if:
- You have a body mass index (BMI) of 40 or more, OR
- Your BMI is between 35 and 39.9 and you have a serious obesity-related health problem
Serious obesity-related health problems include:
- High blood pressure
- High cholesterol
- Type 2 diabetes
- Sleep apnea
- Many others (see Health Benefits section)
For a list of frequently asked questions about qualifying, see our “Do I Qualify For Weight Loss Surgery?” page.
Lap-Band Insurance
SECTION SUMMARY:
- LAP-BAND® surgery is covered by insurance if your policy includes bariatric surgery
In the U.S., the Lap-Band is covered under any plan that includes weight loss surgery, as long as you have:
- Completed a medically supervised diet program
- A body mass index (BMI) over 35 with health problems or over 40 without health problems
If your U.S. insurance covers it, LAP-BAND® surgery deductibles, copays, and coinsurance will cost you about $3,500, depending on your policy. Scroll down this page to learn about the cost of surgery without insurance.
See our Weight Loss Surgery Insurance Guide for everything you need to know about getting insurance to pay as much as possible for your LAP-BAND® surgery.
Click Here to Check Your InsuranceCost of Lap-Band Without Insurance
SECTION SUMMARY:
- The total cost is $15,000, on average (although you may find costs as low as $7,000)
- If you get a medical loan, the loan payment is $334 a month, on average
- You can usually get discounts & tax savings
The average total Lap-Band cost is $15,000. But it can range from $4,000 to $33,000 depending on your location and surgical team. The cost quoted by your surgeon may or may not include pre-op, post-op, complications, or special circumstances, so be sure to ask up front.
Your out-of-pocket costs should be much lower after insurance, discounts, financing, and tax savings are factored in. For example, even if your insurance policy does not cover the LAP-BAND®, some of the expenses may still be covered, such as pre-op testing and lab work.
Click Here to Check Procedure CostFor more cost information:
- See our LAP-BAND® Surgery Cost page
- Free Cost Quote: Click here to contact a LAP-BAND® surgeon
Preparing for Lap-Band Surgery
SECTION SUMMARY:
- If you properly prepare before you have surgery, it reduces your risks during surgery, leads to more weight loss, & saves you money
Your surgeon will work with you during the weeks leading up to your LAP-BAND® surgery, including:
- Encouraging you lose as much weight as possible, because:
- The more weight you lose pre-op, the more weight you will lose after surgery
- The lower your pre-op weight, the lower your risk of complications
- You will regain weight if you slip into old habits. The sooner you can establish good diet and exercise habits, the more likely you will be to maintain them after surgery
- Conducting a health assessment, including questions about your medical history, medications, and surgical history
- Taking steps to stop smoking to reduce your risks of short- and long-term complications
- Ordering certain tests like an ECG, x-ray, and blood tests
- Establishing a pre-surgery diet regimen, including:
- 2 Weeks Before
- No sugar
- Lower carbs
- Increased protein
- Increased veggies
- Plenty of fluids
- 2 Days Before
- Clear liquids, broth, one protein shake per day only
- Talk with your surgeon about whether you should stop taking any medications
- Confirm there are no new medical problems, such as an active infection in your body
- 12 Hours Before
- No food or drink, no tobacco
- 2 Weeks Before
See our Preparing for Weight Loss Surgery page for more information.
Recovery from Lap-Band Surgery
SECTION SUMMARY:
- Hospital Stay: you will be there for 1 day or less
- Time Off Work: you will need 1 to 3 weeks off of work
- Full Recovery: you will be “fully recovered” in 4 to 6 weeks
- Pain: the pain is manageable – it’s same as any laparoscopic surgery
- Diet & Activity: you will slowly transition back to normal
LAP-BAND® surgery patients usually:
- Stay in the hospital for up to one day
- Are back to work in a week or two
Full recovery happens within 6 weeks.
Here’s what you should expect:
- Wake Up. When you first wake up, you’ll be sore and a little “out of it.” You’ll be on medication to control the pain.
- Move Around. Your surgeon will have you up and walking around as soon as possible after you wake up. This will reduce the risk of blood clots and jump-start your body’s healing process. Continue to walk as much as possible, increasing it a little each day.
- Get Released. Before releasing you, your surgical team will run some tests to ensure:
- You are able to drink enough to stay hydrated
- You can urinate normally after removing your catheter
- You have adequate pain relief from your pain medications
- Look for Warning Signs. Contact your surgeon if you experience any of the following:
- Difficulty swallowing
- Fever
- Signs of incision infection (pus, swelling, heat, or redness)
- Ongoing nausea or vomiting
- No improvement or worsening of pain
- Transition Your Diet. Your smaller stomach will be sensitive, especially at first. You’ll start on a liquid diet and slowly transition back to solid foods (read more about this in the Diet section of this page). You may feel tired while your body gets used to less food.
- Ease Off Medications. Your surgeon will prescribe pain and digestion medication as needed. He may also adjust your pre-surgery medications until you’re fully healed. Follow their instructions to the letter.
- Return to Your “New Normal” Life. Avoid swimming or bathing until your incisions have fully healed. Many patients return to normal life and work within a couple of weeks, but plan for up to 4 to 6 weeks off to be on the safe side. Full exercise and heavy lifting should resume within one to two months.
- Have Follow-Up Visits During First Year. Follow-ups with your surgeon’s team will happen about one week post-op, then as-needed to get your band fill amount just right. Every patient is different, but many need 10 or more fill adjustments in the first year before the fill amount is perfect. Fewer adjustments are required as time goes on and your weight stabilizes. Most patients get down to 2 or 3 visits a year by the 3rd year after surgery.
During your follow-up visits, your surgeon will also:
- Adjust your LAP-BAND® as needed by filling/unfilling it via your abdominal port
- Discuss weight loss
- Encourage regular exercise
- Get lab work and make necessary adjustments to medications and dietary supplements
- Understand diet and identify any potential eating disorders
- Determine whether any potential complications may be arising
- Track status of obesity-related health issues
- Involve your family physician to check progress and ensure a successful transition
Lap-Band Diet & Life After
SECTION SUMMARY:
- You will be on a restricted diet with vitamin & mineral supplementation once you have a LAP-BAND®
- You will need ongoing band adjustments
- Your LAP-BAND® might interfere with metal detectors
- You should expect to add regular exercise to your weekly routine to achieve your health and weight loss goals
- Your personal relationships may change
Your weight loss after gastric band surgery is a major part of life after surgery. But it’s also important to consider what day-to-day life will be like.
Your surgery is only a tool. Long-term success requires diligence and sometimes difficult change in other areas, as explained by this Lap-Band patient.
The following sections give you an idea about what changes to expect to your diet and lifestyle before and after surgery. Every surgeon is different, and every patient is different. Please talk with your surgeon before acting on any of the following advice.
1. Food & Drink: Your Diet Transition Schedule
| Timeframe Range | Diet Requirements |
|---|---|
| 2+ Weeks Before Surgery | Practice your gastric band diet |
Recovering from surgery has its own set of challenges. Do not wait until after surgery to start your new life. Establish the following long-term diet habits ahead of time to:
Long-Term Habits to Begin Before Surgery Food
Drinks
Other Habits | |
| 2 Weeks Before Surgery | High protein, low sugar, low carbs |
You will be on a special diet 2 weeks before surgery to reduce the risk of complications. Add the following to the full ‘2+ Weeks Before’ list above:
The typical 2 week pre-op meal plan includes:
The purpose of this diet is to:
| |
| 1 Week Before Surgery | Stop or change some medications |
Your surgeon will ask you to stop taking several medications one week before surgery, such as:
Avoiding these medications will reduce the risk of bleeding and stomach problems after surgery. Consult with your doctor or pharmacist prior to stopping or changing any of your medications. | |
| 2 Days Before Surgery | Clear liquids only |
You should stop eating all foods and drink only clear liquids during the 2 days before surgery. This will clear out your digestive system before surgery. Clear liquids options include:
Do NOT consume:
| |
| Midnight Before Surgery to 7 Days After Surgery (Varies by Surgeon) | Nothing to eat or drink |
Your digestive system must be completely free of food or liquids during surgery. A clean digestive system is especially important for patients with gastroesophageal reflux disease (GERD) or gastric paresis (paralysis of the stomach) (38). When you brush your teeth before heading to the hospital, rinse and spit out the water (don’t swallow). | |
| In Hospital (1 -2 Days) thru Day 7 After Surgery | Clear liquids only |
You will transition into drinking “richer” clear liquids along with the following guidelines:
Drinks that your nurse will provide may include:
Your stomach is in healing mode, so go very easy on it when you return from the hospital. Be sure to drink plenty of fluids, but don’t drink too quickly. Maintain the same clear liquids only diet that you were on in the hospital. Take all vitamins and supplements recommended by your surgeon. If you have no nausea or vomiting, your surgeon may allow you to try thicker items ahead of schedule (see below). Other Habits
| |
| Day 1 to Week 2 After Surgery (Varies by Surgeon) | Add thicker drinks & smooth foods (no chunks) |
Your healing should be well underway. It’s now time to introduce thicker drinks and pureed foods. As soon as you’re ready, your surgeon will start you on many small “meals” per day which may include:
Remember: No soft or solid food and no drinks with chunks or seeds. You can also drink clear liquids between meals. While drinking anything:
| |
| Day 2 to Week 3 After Surgery (Varies by Surgeon) | Slowly test pureed & soft solid foods |
By this point it should be safe to add softer solids to your diet, but take it slow! When you’re ready to start pureed foods, blend water, skim milk, broth, or sugar-free juice with one of the following:
As soon as the pureed foods are going down without a problem, work your way into soft foods like:
And remember those habits you formed in the weeks and months leading up to surgery? Here’s where they start to come in really handy. General diet guidelines during this stage include: Food
Drinks
Other Habits
| |
| Day 3 to Weeks 4+ After Surgery (Varies by Surgeon) | Slowly test solid foods (avoid alcohol) |
Complete your slow transition to your “new normal” long-term diet. Your focus should be on eating your proteins first, in solid form (not protein shakes). Here’s why:
Other points to consider, in addition to those reviewed in Day 2 to Week 3 above, include:
| |
2. Vitamins & Supplements: Your 5 Lifelong Supplements
You will start taking a vitamin regimen for the rest of your life after gastric band surgery. This will help you make up for any nutrients you might not be getting since you eat less with the band.
Here is a list of the vitamins your doctor may ask you to take:
| Vitamins | Main Body System Affected |
|---|---|
| Multivitamin (40) (41) | Entire body |
A daily multivitamin with mineral supplements will help with hair loss and general nutrition problems.
| |
| Calcium (42) | Skeletal |
Calcium citrate supplements will keep your bones strong.
| |
| Folate (folic acid) (43) | Cardiovascular |
Patients who don’t get enough folate are at a higher risk of anemia. For some patients, the folic acid found in a good multivitamin is not enough. Some surgeons do not prescribe extra folate, so ask them to test your folate levels as time goes on to be on the safe side. | |
| Iron (44) (45) | Cardiovascular |
Patients low on iron are more likely to have a stroke, heart attack, or other blood-related problems. In some patients, the iron found in a good multivitamin is not enough. Ask your surgeon to watch your iron levels to avoid any problems. | |
| Vitamin D (46) (47) (48) | Entire Body |
Without enough Vitamin D, you’re at risk of developing rickets, a weakening of the bones, muscles, and teeth.
Talk with your surgeon to be sure, but you may be able to find a calcium supplement that fulfills your Vitamin D requirements. | |
3. Your Ongoing Band Adjustments

It will take time to find the “sweet spot” for your band fill amount. The tighter the band is, the less hungry you feel and vice-versa. Doctors are careful not to over-tighten as that could lead to problems such as reflux and vomiting in addition to preventing you from getting the nutrients you need.
Every patient is different, but it is not uncommon to need 10 or more fill adjustments before finding the perfect fill amount in the first year.
As time goes on and your weight stabilizes, you’ll need fewer adjustments. By year 3 you should need no more than 2 or 3 adjustments per year.
When it comes to getting your fill “just right,” trust your instincts and push back if your doctor continues to recommend fill/unfill amounts that aren’t working for you. For example, some doctors insist upon adding or removing at least 0.50 cc’s with each visit, but your body may require tiny 0.25 cc adjustments instead.
For an interesting discussion about getting the fill amount just right, see this patient back-and-forth about getting a perfect gastric band adjustment.
4. Interference with Metal Detectors & Other Equipment
Metal Detectors – Probably no problems
Your band will probably not interfere with external equipment like airport metal detectors, although it can happen. It depends on the sensitivity of the metal detectors and how much other metal you are carrying with you (since the detectors will only go off if the total metal you are carrying exceeds a certain amount).
Metal Detecting Wand – May cause problems
A metal detecting wand will detect your port, so play it on the safe side and carry a note or card from your doctor identifying you as a gastric band patient.
MRI machines – No problems
Your gastric band should not interfere with MRI devices, but let your MRI doctor know about your band to be on the safe side.
5. Exercise: you should exercise 2.5 hours per week, spread out over 2 to 4 days
Exercise with a gastric band is almost as important as your diet when it comes to long-term success:
- Patients who exercise regularly lose more weight over the long-term
- Physical and mental health benefits are incredible
How much exercise do you need to for noticeable results?
One study of gastric bypass patients found that 2.5 hours per week resulted in 5.7% greater excess weight loss (49). Gastric band patients should expect similar results.
To help you stay on track, block out time to exercise at the same times on the same days of the week.
Also, spread your 2.5 hours per week out over 3 or 4 days (in other words, 30 to 45 minutes 3 or 4 days per week). This will make it less intimidating to get started each day and will help you build endurance.
Exercise Types: 3 Goals
There should be 3 main goals of your exercise routine:
- Endurance – walking, stationary bike, and especially swimming
- Flexibility – a good stretching routine. Yoga is best since it incorporates proper breathing and uses your own body weight to build strength
- Strength – exercise balls, weights, and yoga
Learn more about exercise after weight loss surgery.
6. Your Brain: Less Hungry, Careful About Food Addiction, New Mentality Will Change Behavior & Relationships
Food Addiction
Our bodies secrete certain hormones (like ghrelin) that tell us when we’re hungry. Junk food may override those hormone signals by overstimulating our reward centers. This is just like the way our bodies and brains react to an addictive drug.
You may have food addiction if your desire for food takes priority over other important parts of your life, such as:
- Personal health
- Family
- Friends
- Work
- Your appearance
- Avoiding obesity related health issues like hypertension, sleep apnea, or diabetes
If left unchecked, food addiction can lead to obesity. If not addressed before surgery, it can also lead to weight regain.
To find out if you may be suffering from food addiction, take our Food Addiction Quiz.
Relationships After Weight Loss
Being thin again, or being thin for the first time, may be a shocking experience. Many gastric band patients express amazement at:
- No more obesity discrimination. For example, strangers tend to be nicer to thin people.
- Being treated with more respect
- Getting more romantic interest from others
- Building deeper relationships by being able to physically keep up with kids and more physically fit friends
- Getting more compliments from others
- Increased self-confidence and the effect that has on others
- Improvements in quality of sexual life (50)
But there may be negatives to being thin as well.
People who you’ve known for a long time will not be used to the way you look and may not know how to act around you. For example:
- How will overweight friends or family members feel when you’re losing weight but they are not?
- Will your new healthier diet and smaller portion sizes make meals with others awkward?
- Could intimacy with your spouse or partner be affected?
- Could your spouse or partner become jealous now that others are noticing you more?
- How will your coworkers react? Should you even tell them you are having surgery?
- Will your friends or family make it difficult for you to stay on track by making bad diet choices?
- Could your new self-confidence create conflict with people who are used the “old” you?
And what about the new “skinny lens” you see the world through? For example:
- Would this person be treating me the same way if I hadn’t lost all this weight?
- How do I handle obesity discrimination now that I’m on the “other side”?
Be prepared for both the good and the challenging “shocks” of dramatic weight loss following surgery.
For real life experiences and advice from other patients, see our Relationships After Weight Loss surgery page.
Lap-Band Risks & Downsides
SECTION SUMMARY:
- There is a moderate risk of non-serious complications
- You might have to have your LAP-BAND®removed eventually, as is required in up to 50% of patients
- You may experience side effects, including digestion issues & sagging skin from rapid weight loss
- It is possible that you will regain some weight
Historically, 30+% of LAP-BAND® surgery patients eventually required band removal (51). However, recent studies have shown the 5-year removal rate drop to under 9% for patients who maintain continued interaction with their surgical team and follow established guidelines closely (52).
Possible Complications
Gastric band removal required in about 9% of patients by 5 years post-op due to inadequate weight loss or one of the following complications:
- Band problems: 1.1% – 18% of patients
- Esophageal dilation: 14% of patients
- Food trapping: 1 to 2% of patients
- Port problems: 20.5% of patients
- Pouch dilation: 6.3% – 16.9% of patients
Possible Side Effects
- Intolerance to certain foods may cause nausea, vomiting or indigestion. Fixed by changing diet or eating habits.
- Digestive issues, such as the feeling of food getting stuck after eating too quickly or not chewing your food enough.
- Bowel function changes, including constipation or diarrhea, are also usually fixed by patient diet adjustments.
- Sagging skin as a result of rapid weight loss
- Weight regain possible if don’t change diet & lifestyle
For more information about potential downsides, see our Lap Band Complications & Side Effects page.
How Does the Lap-Band Compare to Other Weight Loss Procedures?
SECTION SUMMARY:
- The LAP-BAND® is one of the best procedures for weight loss & health improvement
- The amount of weight loss varies more from patient to patient
- It is one of 4 procedures that is reversible, and it results in the most weight loss among reversible procedures by far
- It is 1 of 4 procedures that results in 50%+ average excess weight loss (EWL)
- The LAP-BAND® has the highest long-term ‘failure’ rate among 50%+ EWL procedures
Gastric band surgery used to be the 2nd most popular procedure. Although it has a number of good reasons to consider it, its popularity dropped significantly because research showed a high rate of long-term complications that required removal of the band.
However, that trend may be changing as a result of recent studies that have shown big drop in removal rates when patients maintain continued interaction with their surgical team and follow established guidelines closely (53).
1. Gastric Band Surgery Positives
- Weight loss is usually better than gastric balloon (but less than gastric sleeve, gastric bypass, or duodenal switch). However, weight loss after gastric band surgery is highly variable. It ranges from 20% (similar to gastric balloon) to 80% (similar to duodenal switch). More research is needed for the AspireAssist, but initial results show about 30% weight loss on average.
- Health Improvement is generally better than after gastric balloon (but not as good as gastric sleeve, gastric bypass, or duodenal switch). Initial research for the AspireAssist shows similar heath improvements to gastric balloon, but more research is needed to confirm this result.
- Reduced hunger – only gastric sleeve and duodenal switch make you feel less hungry.
- Short-term risk of gastric band surgery complications is lower than duodenal switch, gastric sleeve, and gastric bypass (but higher than gastric balloon or AspireAssist).
- Adjustable – As time goes on, the tightness of the band can be adjusted for each patient to find the “perfect” level of tightness. The Spatz gastric balloon (not available in the U.S.) is the only other procedure that is adjustable after surgery (the Orbera, ReShape, and Obalon gastric balloons are not adjustable).
- Reversible – Gastric band surgery, along with gastric balloon and AspireAssist, is reversible. This means that if you don’t like it, you can go back to the way things used to be or try another procedure. Gastric sleeve, gastric bypass, and duodenal switch surgery are not reversible – once your stomach size is reduced and your intestines are rerouted, it is very difficult and uncommon for those procedures to be reversed.
- Hospital Stay – Usually shorter with gastric band (1 day) than with gastric sleeve, gastric bypass, or duodenal switch (2 to 3 days) (but generally longer than gastric balloon and AspireAssist which are done on an outpatient basis).
- No dumping syndrome – Dumping syndrome is experienced by up to 7 out of 10 gastric bypass patients, although many patients report this being a “good thing” since it helps them keep their diet on track.
- Cost With Insurance is tied for the lowest with gastric sleeve, gastric bypass, and duodenal switch (gastric balloon and AspireAssist usually are not covered by insurance).
- Cost Without Insurance – If you do not have insurance that covers weight loss surgery, the Lap-Band has the 2nd lowest overall cost (gastric balloon is lowest). It has the lowest total cost of the “permanent” procedures (gastric balloon is less expensive but must be removed after 6 months).
- Vitamin Regimen – since the gastric band procedure is primarily “restrictive” in nature (makes you feel full sooner), there is a lower risk of vitamin and mineral deficiency than after gastric bypass or duodenal switch (vitamins will be similar to gastric sleeve and gastric balloon).
2. Gastric Band Surgery Negatives
- Weight loss is usually not as good as gastric sleeve, gastric bypass, or duodenal switch (but is likely better than gastric balloon). The AspireAssist needs more research, but early results suggest weight loss similar to gastric balloon.
- Health Improvement is generally not as good as gastric sleeve, gastric bypass, or duodenal switch (but is likely better than after gastric balloon). Initial research suggests the AspireAssist will have similar health benefits to gastric balloon, but more research is needed to confirm.
- Hunger Will Remain the Same – Gastric band surgery will not change how hungry you feel, only how much you can eat. Gastric sleeve and duodenal switch cause patients to also feel less hungry due to fewer hunger-causing hormones being released or by blocking hunger signals sent to the brain.
- Short-term risk of gastric band surgery complications is higher than gastric balloon or AspireAssist (but lower than duodenal switch, gastric sleeve, and gastric bypass).
- Long-term risk of gastric band surgery complications is relatively high. About 9% of Lap-Band patients must eventually have their band removed (54).
- External device used – There is an external device left inside the body which opens up the risk of device-related complications. While the risk of device-related complications is relatively low for gastric balloon and AspireAssist, it is a concern and should be considered for gastric bands.
- Hospital Stay – Gastric band surgery usually requires one day in the hospital vs in and out the same day (outpatient) with gastric balloon and AspireAssist (but gastric band hospital stays are usually shorter than with gastric sleeve, gastric bypass, or duodenal switch (2 to 3 days)).
- Recovery Time – You should allow about 2 weeks before returning to work after gastric band, gastric sleeve, gastric bypass, and duodenal switch. Gastric Balloon and AspireAssist patients usually return to work in a few days.
- Follow-Up Visits – One of the benefits of the band is that it is adjustable. The downside of being adjustable is that it can be difficult to find a “band fill amount” that is just right. This means many visits to the doctor – up to 10 or more in the first year – to fill and unfill the band before finding the “perfect” level of constriction. The patient may experience discomfort until this level is found, especially if the band is too tight (too full).
For a complete comparison of all procedures, see our Types of Bariatric Surgery page.
Click Here for a Summary of All ProceduresLap-Band Surgery Summary
SECTION SUMMARY:
- 7 steps to your long-term weight loss using the LAP-BAND®
1. Start Working with a Weight Loss Surgeon As Soon as Possible
Surgeons will help you navigate your surgical options, pre-surgery steps, financing, and insurance options:
- Many surgeons offer a free initial consultation, free local seminar, or free webinar. These will give you a better idea of what to expect and allow you to ask questions.
- Many also provide a free insurance check. They will also help you appeal any denials or find financing.
- Most insurance companies need proof of a medically supervised diet program. Your surgeon will set this up for you if you haven’t done so already.
- Your surgeon will push you towards new habits that will be essential to success after surgery. Many surgeons will recommend support group meetings for feedback from actual patients.
2. Two Weeks Out: Prepare for Surgery
You will have completed your pre-op tests, physical, and any other required steps. You should have insurance approval by this point. You should also be well on your way towards developing your diet and lifestyle habits.
In the week or two leading up to surgery, you’ll go to the hospital pre-surgery department. They will perform an EKG, blood work, and any last minute tasks or other pre-op tests. You’ll meet with the surgeon one more time to wrap up final tests and forms. The night before surgery, do not eat or drink anything starting at midnight.
3. Surgery Day
You’ll arrive at the hospital at least two hours before surgery to allow for prep time. The Lap-Band procedure itself will take about 1 hour to perform. Immediately after surgery, you’ll have a dedicated nurse to manage your pain and check your vitals.
4. Recovery
Most Lap-Band patients are in the hospital for 1 day. You can’t eat or drink anything for at least 24 hours after surgery. And your surgeon will want you to get up and walk around as soon as possible to start the healing process. You’ll leave as soon as your surgeon is confident that you are well on the road to full recovery. You’ll need someone to drive you home from the hospital and care for you for at least a few days following surgery. Full recovery generally happens within 2 to 4 weeks.
5. Adjust to Your New Post-Surgery Diet & Lifestyle
For the first 4 to 5 weeks after surgery, you will go from a clear liquid diet to your “new normal” Lap-Band diet. You should also continue your transition into a more active lifestyle. You will feel full sooner after eating and start to experience weight loss within a couple weeks.
Your surgeon’s dietitian or nutritionist will help you determine an appropriate diet. See the Diet & Life After section of this page for more information.
6. Attend Support Groups Regularly
Regular support group participation leads to:
- Reduce post-op recovery time
- Lead to as much as 12% more long-term weight loss
Your surgeon will be able to recommend an in-person group near you.
7. Ongoing Doctor Visits
Your surgeon will schedule a follow up visit within 2 weeks to ensure you are recovering well and to answer any questions.
You will continue to meet with your surgeon during the first year in order to adjust your band.
Your surgeon will inject saline solution into your band through the port located just under the skin of your abdomen. You will continue to add and remove saline solution through the port (“fill” and “unfill” the band) until the perfect balance is found, which may require 10 or more follow-up visits in the first year.
In year 2, most patients need 4 to 6 adjustments. Every year thereafter, 2 or 3 adjustments are usually enough.
After the perfect fill amount is found, you should meet with your surgeon at least once a year for check-ups and stay in close contact with your surgeon’s dietitian.
Find a Weight Loss Surgeon
SECTION SUMMARY:
- You can ask a local bariatric practice for a free insurance check or cost quote
- You can attend a free in-person seminar or an online webinar offered by a local weight loss surgeon
- You should schedule a phone or in-person consultation (both often free), if you are interested in learning more about weight loss surgery
Search the Lap-Band Surgeon Directory below to find a weight loss surgeon by country and region: