There are 6 types of weight loss surgery (also called “bariatric surgery”) available. Each type has advantages and disadvantages, and this page will help you decide which one is right for you.
Here is a very brief description of how each procedure will help you lose weight:
- Gastric Sleeve – you will feel less hungry generally & full sooner while eating
- Gastric Bypass – you will feel full sooner while eating & absorb fewer minerals
- Duodenal Switch – you feel less hungry generally & full sooner while eating, absorb fewer calories and minerals
- LAP-BAND® – you will feel full sooner while eating
- Gastric Balloon – you will temporarily feel full sooner while eating (balloon removed after 6 months)
- AspireAssist – drain a portion of stomach contents after eating and absorb fewer calories
TABLE OF CONTENTS
Click on any of the topics below to jump directly to that section
- Procedure Summaries
- Weight Loss
- Health Improvement
- How to Qualify
- Insurance
- Cost Without Insurance
- Recovery
- Diet & Life After
- Risks & Downsides
- Summary: Best Weight Loss Procedure By Category
- Test Your Knowledge
- Find a Weight Loss Surgeon
Weight Loss Surgery Procedure Summaries
SECTION SUMMARY:
- Some procedures reduce the amount of food you can eat
- Some make you feel less hungry
- Some reduce the amount of minerals and/or calories that your body can absorb
Following are overviews of each of the 7 available types of weight loss surgery, including how they work and how they will help you to lose weight quickly.
Gastric Sleeve
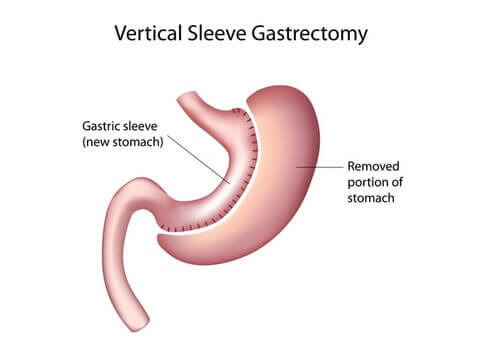
If you choose gastric sleeve:
- A big portion of your stomach will be removed
- You will feel full sooner after eating
- You will lose weight quickly because:
- You will not be able to eat as much
- Your smaller stomach will secrete fewer hunger-causing hormones which means you won’t feel as hungry
Tap here for more information about gastric sleeve surgery
Gastric Bypass
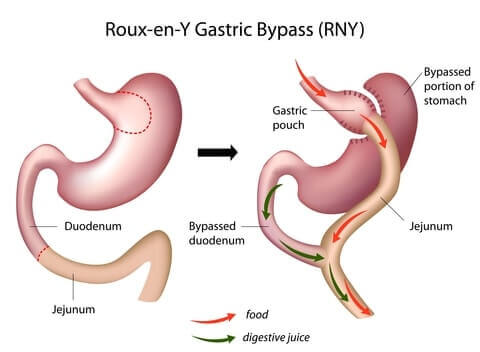
If you choose gastric bypass:
- Your stomach will be split into 2 parts: a small pouch at the top and the rest at the bottom
- Your intestines will be rearranged to bypass the the top portion of your small intestines
- If you do not follow a strict diet, you will have problems with malnutrition and dumping syndrome
- You will lose weight quickly because:
- Your smaller stomach pouch will cause you to feel full sooner while eating
- You will not be able to eat as much
- Your body will absorb fewer minerals
Tap here for more information about gastric bypass surgery
Duodenal Switch
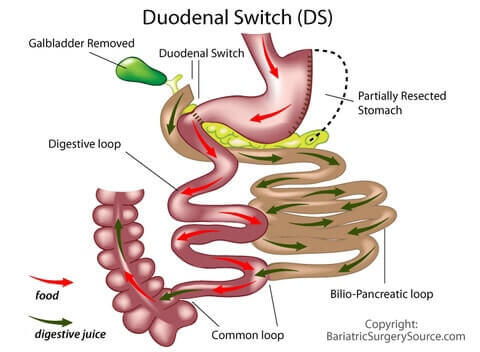
If you choose duodenal switch:
- A big portion of your stomach will be removed
- Your intestines will be rearranged to bypass a long portion of your small intestines
- Your gallbladder will be removed
- You will feel full sooner while eating
- You will lose weight quickly because:
- Your smaller stomach will secrete fewer hunger-causing hormones which means you won’t feel as hungry
- Your body will absorb fewer minerals and calories
Tap here for more information about duodenal switch surgery
LAP-BAND®
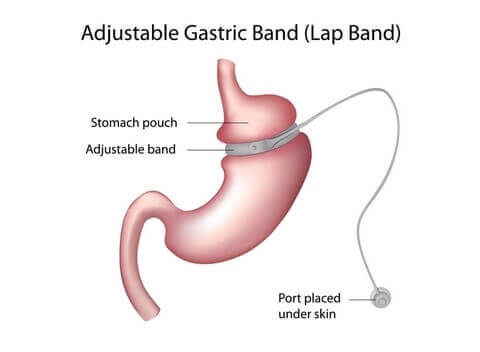
If you choose LAP-BAND®:
- An adjustable band will be wrapped around the top portion of your stomach, creating a small stomach “pouch” above the band.
- Your smaller stomach pouch will fill up quicker while eating
- You will lose weight quickly because you will not be able to eat as much
Tap here for more information about LAP-BAND® surgery
Gastric Balloon
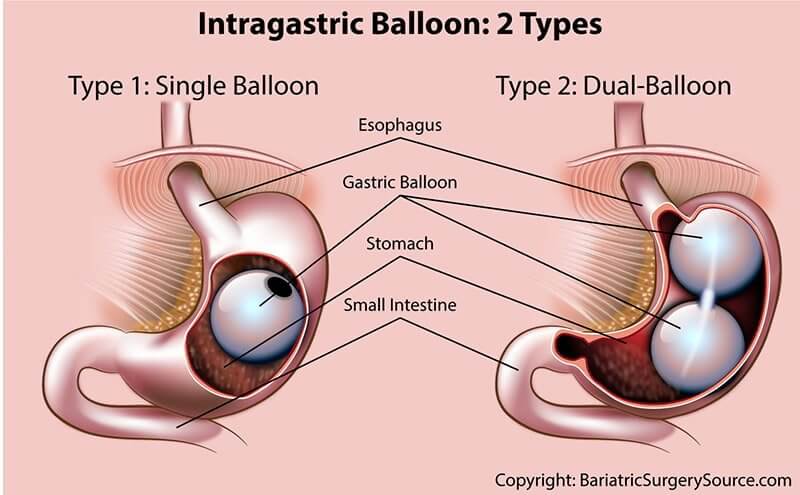
There are currently 2 types of gastric balloons available in the United States: single balloon (which may include multiple single balloons, depending on the balloon manufacturer) and dual-balloon. If you choose one of these procedures:
- A deflated balloon will be inserted into your stomach through your mouth, then will be inflated once it reaches your stomach
- You will lose weight because you won’t be able to eat as much
Tap here for more information about the gastric balloon procedure and options
Aspire Assist

If you choose the AspireAssist device:
- Your stomach will be connected to a port on the outside of your abdomen
- After each meal, you will connect a tube and pump to your abdominal port and empty part of your stomach contents
- You will lose weight because a large portion of your meals will be removed from your stomach before your body has a chance to digest and absorb it.
Tap here for more information about the AspireAssist device
Weight Loss After Bariatric Surgery
SECTION SUMMARY:
- You will lose 25% to 90% of your excess weight, depending on the procedure you choose
- If you’re 5’ 4” tall and weigh 240 lbs, that means you’ll lose 24 – 86 lbs
- If you’re 5’ 9” tall and weigh 300 lbs, that means you’ll lose 33 – 119 lbs
- It usually only takes between 12 and 18 months to reach your low weight
- More complex procedures generally result in the most long-term weight loss
You will lose weight quickly after most procedures, with your low weight coming 12 to 18 months after the procedure.
At 65% to 70% excess weight loss after 1 year, the duodenal switch (DS), gastric sleeve, and gastric bypass are very similar. The DS pulls ahead over the long-term as you’ll be less likely to gain weight back after the first couple of years.
At 40% excess weight loss after 1 year, Lap-Band is 4th behind sleeve, bypass, and DS.
Gastric balloon and AspireAssist are at the low end of the weight loss spectrum at 25% – 30% excess weight loss after 1 year.
Use the button below to compare average weight loss over time for each procedure and to project your weight loss with each procedure.
Click Here to See How Much Weight You Could LoseProcedure Award: Most Weight Loss
- Winner: Duodenal Switch
- Runners Up: (Tie) Gastric Sleeve & Gastric Bypass
Health Improvement After Weight Loss Surgery
SECTION SUMMARY:
- You could cure or drastically improve your diabetes, sleep apnea, hypertension, and at least 12 other conditions, depending on the procedure
All types of bariatric surgery have proven health benefits. Some are preventative, like the risk of cancer reducing by 33% after surgery (1). Others help you move, like a 4 pound reduction in pressure on the knee joint for every pound of weight lost (2).
The duodenal switch (DS) is the clear front-runner in terms of health improvement. In fact, DS surgery is even being performed on non-morbidly obese patients to treat metabolic syndrome and diabetes (3).
It works so well because it combines the restriction of gastric sleeve, making patients feel full sooner after eating, with its own brand of malabsorption to limit the number of calories that the body can absorb.
Despite its effectiveness, most surgeons tend to only consider it for super-obese patients (BMI of 50 or greater) because:
- It is more difficult to perform
- It takes longer to perform
- It requires much more diligent follow up for both surgeons and patients due to the the level of malabsorption that it causes
While not as good as the DS, gastric sleeve and gastric bypass have extremely impressive health improvement stats as well.
| Co-morbidity | Gastric Balloon % Improved /Resolved | Gastric Sleeve % Improved /Resolved | Bypass % Improved /Resolved | DS % Improved /Resolved | Band % Improved /Resolved | AsipreAssist % Improved/ Resolved |
|---|---|---|---|---|---|---|
| Dyslipidemia hypercholesterolemia | 10% | 64% | 63% | 99% | 70% | |
| Diabetes | 33% | 55% | 83% | 92% | 60% | Possible improvement |
| Hyperlipidemia (high levels of fat in the blood, high cholesterol) | 34% | 35% | 73% | 99% | 23% | Possible improvement |
| High Blood Pressure (hypertension) | 45% | 68% | 69% | 83% | 43% | Possible improvement |
| Joint/Bone Disease (osteoarthropathy) | 48% | 46% | 43% | 43% | 81% | |
| Depression | Most | Most | Most | 57% | ||
| Migraines | 40% | 57% | Most | Some | ||
| Pseudotumor cerebri | n/a | 96% | – | Most | ||
| Cardiovascular Disease | 100% | 79% | 86% | 73% | ||
| Venous Stasis Disease | 95% | 95% | – | – | ||
| Gastroesophageal Reflux Disease (GERD) | 50% | 80% | 49% | 87% | ||
| Non-Alcoholic Fatty Liver Disease | n/a | 90% | 99% | Most | ||
| Mortality Reduction/ Life Expectancy (5 year mortality) | 89% | 89% | 89% | 89% | ||
| Quality of Life Improvements | 93% | 95% | 95% | Most | ||
| Metabolic Syndrome | 62% | 80% | 99% | 70% | ||
| Polycystic Ovarian Syndrome | Most | Most | Most | 48% | ||
| Pregnancy | Most | Most | – | Most | ||
| Asthma | 90% | 80% | 90% | – | ||
| Obstructive Sleep Apnea | 62% | 98% | 99% | 85% | ||
| Stress Urinary Incontinence | 90% | 88% | – | 82% | ||
| Reduced Cancer Risk | – | 33% | 33% | 33% | 33% |
Procedure Award: Best Health Improvement
- Winner: Duodenal Switch
- Runners Up: (Tie) Gastric Sleeve & Gastric Bypass
How to Qualify for Weight Loss Surgery
SECTION SUMMARY:
- Your body mass index (“BMI”) needs to be at least 30 to qualify for a weight loss procedures
- The more complex procedures require a BMI of at least 35
In order to qualify for any type of weight loss surgery, your body mass index (BMI) must fall within a certain range.
The following procedures have a limited acceptable range:
- Gastric balloon: Accepts BMIs from 30 to 40
- AspireAssist: Accepts BMIs from 35 to 55
The rest of the procedures (gastric sleeve, gastric bypass, duodenal switch, and gastric banding) have the same qualification requirements:
- Body mass index 40 or above or
- Body mass index from 35 to 40 as long as you have a serious obesity-related health problem (“comorbidity”) such as diabetes, asthma, hypertension, joint problems, sleep apnea, or one of many others.
- Body mass index from 30 to 35 may be accepted if certain health issues are present
For a list of frequently asked questions about qualifying, see our “Do I Qualify For Weight Loss Surgery?” page.
Procedure Award: Easiest to Qualify
- Winner: No Clear Winner (it depends on your height and weight)
Weight Loss Surgery Insurance
SECTION SUMMARY:
- Gastric sleeve, gastric bypass, Lap-Band, and duodenal switch will be covered by insurance if your insurance policy includes bariatric surgery
- Gastric balloon and AspireAssist are not usually covered by insurance
- Your surgeon may be able to get some of your costs covered, even if your policy does not include bariatric surgery
If your insurance policy includes weight loss surgery, four procedures will be covered:
- Gastric sleeve surgery
- Gastric bypass surgery
- Duodenal switch surgery (biliopancreatic diversion with duodenal switch)
- Gastric banding (LAP-BAND® surgery)
The weight loss surgery insurance approval process can take anywhere from 1 to 12 months, depending on your insurance company and your situation.
Fortunately, your surgeon’s office will do most of this legwork for you. They will be highly experienced in managing the process and may even have all of the required personnel on staff (e.g. registered dietitian, psychiatrist, bariatric coordinator, etc.).
Click here to access the weight loss surgeon directory to get started. Most offices will do a free check of your insurance policy to see if it covers weight loss surgery.
For more information about weight loss surgery insurance, see our Bariatric Surgery Insurance Guide.
Procedure Award: Insurance Coverage
- Winner: (4-Way Tie) Sleeve, Bypass, Band, & Duodenal Switch (because if one is covered, all are covered)
Cost of Weight Loss Surgery Without Insurance
SECTION SUMMARY:
- If your insurance does not cover bariatric procedures, your out-of-pocket costs will range from $4,000 to $27,000 depending on the procedure and surgeon you choose
- You may be able to get a loan to cover the costs if your credit score is at least 650
- Self-pay discounts and tax savings are usually available
The cost of surgery should not dictate which procedure you have. Through research and consultation with your surgeon, you should move forward with the procedure that is most likely to work for you.
Still, if you don’t have insurance that covers bariatric surgery, it’s important to know what you’re up against financially.
Click Here to Check Procedure CostThere are a few key points to consider:
- Actual costs vary widely depending on the region, hospital, and surgeon.
- Quoted costs may not be all inclusive. Talk with your surgeon or hospital for a more specific quote.
- Long-term costs will probably be much lower for the more expensive procedures. Even though they are not declared “Low-Cost Winners” in this section, the more expensive procedures tend to do a much better job at improving or resolving obesity-related health problems which will save you more money over the long-term. More on this in the “Cost of Not Having Surgery” sub-section below.
Regardless of which procedure you choose, financing is available to many patients to help make surgery more affordable (requires a minimum credit score of 650).
Please visit our Financing Weight Loss Surgery page for all the possible ways to finance your surgery.
Procedure Award: Low-Cost Procedure (Without Insurance)
- Winner: Gastric Balloon (but long-term costs likely higher than more expensive procedures)
- Runner Up: LAP-BAND®
Procedure Award: Low-Cost Procedure (With Insurance)
- Winner: 4-Way Tie – Gastric Sleeve, Gastric Bypass, Duodenal Switch, & LAP-BAND®
- Runner Up: Gastric Balloon
Cost of Not Having Surgery vs. Cost of Weight Loss Surgery
The cost of any procedure is far less than the long-term costs of obesity-related health problems for morbidly obese people who don’t have surgery.
In fact, weight loss surgery patients pay off their entire surgery and start getting ahead financially after only 2 years (4).
Fewer prescription drugs alone have been found to save patients $3,000 or more per year (5).
Recovery from Weight Loss Surgery
SECTION SUMMARY:
- You will be in the hospital from 0 to 3 days, depending on the procedure
- You’ll need to take between 2 days and 2 weeks off of work, depending on the procedure
- You will fully recover in 3 days to 6 weeks, depending on the procedure
The amount of time you’ll spend in the hospital and the recovery time depends on how complicated your procedure is (whether part of the stomach is removed or digestive system rearranged, etc).
Less Complicated Procedures
- Gastric balloon
- AspireAssist
The less complicated procedures, including gastric balloon, and AspireAssist have the shortest hospital times (return home the same day as surgery) and recovery times (back to work in 3 to 4 days).
More Complicated Procedures
- LAP-BAND®
- Gastric sleeve
- Gastric bypass
- Duodenal switch
The moderately complicated procedure, LAP-BAND®, will require a 1 day hospital stay and will have you back to work in 2 weeks.
More complicated procedures, including gastric sleeve, gastric bypass, and duodenal switch, typically require 2 to 3 days in the hospital, although you should still be able to return to work within 2 weeks.
Procedure Award: Quickest Recovery
- Winner: (Tie) Gastric Balloon and AspireAssist
- Runner Up: LAP-BAND®
To learn all about what to expect during your recovery, see our Bariatric Surgery Recovery page
Weight Loss Surgery Diet & Life After
SECTION SUMMARY:
- Your new diet will range from “no restrictions” to “restricted with supplementation”, depending on the procedure you choose
- You should expect to add regular exercise to your weekly routine
- You should feel much less hungry and/or full sooner while eating
- If you suffer from Food Addiction, you may still struggle after surgery
- Your personal relationships will probably change
The “best” long-term diet after weight loss surgery means different things to different people. For example, “best” to you could mean:
- Most weight loss, regardless of sacrifices
- Fewest long-term diet changes, even if less weight loss
- Anywhere in between
Unfortunately, you can’t have it all, so the following sections provide an overview of what to expect after each procedure.
Food & Drink
Gastric balloon and AspireAssist have their own guidelines and tend to be much less stringent.
The more complicated procedures, including gastric sleeve, gastric bypass, duodenal switch, and LAP-BAND®, have very similar diet requirements before and after surgery.
Generally speaking, your new diet after these procedures will feel very healthy and regimented, including:
- Mainly “whole” foods (meat and vegetables)
- Plenty of protein
- No processed foods
- Minimal sugar or sugary drinks
- No dairy
- No starchy foods like rice, bread, and pasta
- No fibrous foods that are tough to digest like celery, nuts, and tough meats
- Plenty of fluids, but not around meal time
- Minimal alcohol
Our Bariatric Diet page includes all of the specifics.
Procedure Award: Best Post-Op Diet
Winner: Depends on your weight loss goals (your willingness to accept a more stringent diet will lead to more weight loss)
Vitamins & Supplements
Since you will be eating less after any type of weight loss surgery, you will likely bariatric-diet.htmlneed to supplement your diet with a daily multivitamin a daily calcium supplement:
All surgical procedures (sleeve, bypass, band, and DS) will require additional supplementation.
See our Bariatric Vitamins page for more information.
Exercise
Following recovery, exercise should be the same for all procedures: 2.5 hours per week, spread out over 2 to 4 days. Keep in mind that patients who exercise regularly:
- Lose more weight
- Are more physically and mentally healthy
Learn more on our Exercise After Weight Loss Surgery page.
Reduced Hunger
You will probably feel less hungry after gastric sleeve and duodenal switch.
When your stomach is empty, it secretes a hormone called ghrelin into your bloodstream which causes your brain to generate hunger impulses. After you eat, the amount of secreted ghrelin drops then slowly rises until your next meal. Since your stomach will be significantly smaller following these gastric sleeve and duodenal switch, the amount of ghrelin the stomach secretes – and your resulting feelings of hunger – should also go down.
The other procedures leave the stomach in place and do not utilize a hunger-blocking device, so changes to hunger will remain largely unaffected.
Food Addiction
Regardless of which procedure you have, food addiction could be a problem.
Your body secretes certain hormones, like ghrelin mentioned above, that tells us when you’re hungry and full. Hyperpalatable food (like junk food) may be overriding those hormone signals by overstimulating our reward centers, much like our bodies and brains react to an addictive drug.
You may have a bona fide food addiction if your desire for food takes priority over other parts of your life that you acknowledge to be more important, such as personal health, family, friends, work, your appearance, or avoiding obesity related health issues like hypertension, sleep apnea, or diabetes.
If left unchecked, food addiction can lead to obesity. For weight loss surgery patients, if not addressed prior to surgery, it can also lead to weight regain.
To find out if you may be suffering from food addiction, take our Food Addiction Quiz.
Relationships
Significant weight loss after any type of bariatric surgery can lead to big changes with everyone around you.
While many of those changes are positive, some can also be extremely challenging and unexpected.
See our Relationships After Weight Loss Surgery page for important changes to prepare for.
Weight Loss Surgery Risks & Downsides
SECTION SUMMARY:
- There is a low to moderate risk that you’ll experience a non-serious complication
- Side effects may include digestion issues & sagging skin from rapid weight loss
- You will eventually regain weight if you do not stick to your new diet and exercise plan
Complications
First, weight loss surgery is almost never life-threatening. Unlike the horror stories you may have heard during the early days of bariatric surgery, the survival rate is now up to 99.9%.
However, the types of bariatric surgery that result in more weight loss (sleeve, bypass, band, and DS) are often accompanied by higher risk of non-life-threatening complications and additional lifestyle changes.
See our Bariatric Surgery Complications page for more details.
Digestion Issues
Digestion issues are possible after all procedures. Depending on the procedure, they may include:
- Intolerance to certain foods
- Bowel movement problems
- Difficulty swallowing
- Indigestion
- Nausea and vomiting
- Vitamin and mineral deficiency
Dietary adjustments will usually fix any digestion issues that may come up.
Sagging Skin
Sagging skin is an issue for most patients who lose a lot of weight quickly, especially after gastric sleeve, gastric bypass, duodenal switch, and LAP-BAND®.
It is less likely after gastric balloon because patients tend to not lose as much weight after those procedures.
Weight Regain
5% to 10% percent weight regain is common after most procedures, although it is much less likely after duodenal switch surgery due to that procedure’s unique combination of restriction and malabsorption.
Weight regain is usually the result of patients not following proper diet guidelines.
Weight Loss Surgery Summary: Best Procedure By Category
SECTION SUMMARY:
- See below for the best procedure by category
Your individual situation will determine which type of bariatric surgery is best for you. Unfortunately, there is no “one size fits all” option. Following is a review of winners in each category:
Most Weight Loss
- Winner: Duodenal Switch
- Runners up: (Tie) Gastric Sleeve & Gastric Bypass
Best Health Improvement
- Winner: Duodenal Switch
- Runners up: (Tie) Gastric Sleeve & Gastric Bypass
Easiest to Qualify
- Winner: No Clear Winner; Depends on Your Current BMI
Low-Cost Procedure (Without Insurance)
- Winner: Gastric Balloon (but long-term costs likely higher than more expensive procedures)
- Runner up: Lap Band (but long-term costs likely higher than more expensive procedures)
Low-Cost Procedure (With Insurance)
- Winner: 4-Way Tie – Gastric Sleeve, Gastric Bypass, Duodenal Switch, & LAP-BAND®
- Runner up: Gastric Balloon
Insurance Coverage
- Winner: (4-Way Tie) Sleeve, Bypass, Band, & Duodenal Switch
Most Popular Procedure
- Winner: Gastric Sleeve
- Runner up: Gastric Bypass
Quickest Recovery
- Winner: (Tie) Gastric Balloon and AspireAssist
- Runner up: LAP-BAND®
Best Post-Op Diet
- Winner: Depends on Patient’s Goals; Easier Diet’s Usually Mean Less Weight Loss
Fewest Risks & Side Effects
- Winner: (Tie) Gastric Balloon & Gastric Sleeve
- Runners up: The AspireAssist
Overall Winner for You Depends on Your Goals
- Winner: Take the Choose My Procedure Quiz
- Runner up: Take the Choose My Procedure Quiz
If you’re still on the fence between two procedures, these pages will help you understand the differences:
Test Your Weight Loss Surgery Knowledge
Types of Weight Loss: Test Your Knowledge

Well-educated patients are more likely to be successful over the long-term. Test your knowledge to ensure that you’re ready to take the next step!
Find a Weight Loss Surgeon
SECTION SUMMARY:
- You can ask a local bariatric practice for a free insurance check or cost quote
- You can attend a free in-person seminar or an online webinar offered by a local weight loss surgeon
- You should schedule a phone or in-person consultation (both often free), if you are interested in learning more about weight loss surgery




