Roux en Y gastric bypass surgery is successful for the majority of patients, but gastric bypass revision surgery may be necessary if you experience significant weight regain after hitting your low weight (1).
Review the information below and click the sections to find out if revision surgery is right for you.
TABLE OF CONTENTS
Click on any of the topics below to jump directly to that section
Is Revision Surgery the Best Choice?
SECTION SUMMARY:
- Rule out diet & exercise issues
- Check stomach pouch stretching
- Check stoma size (opening to small intestine)
- Check other causes of weight regain
The most common reason patients consider gastric bypass revision is weight-related… either not enough was lost following surgery or too much was gained back (2).
Research shows that up to 20% of patients who were morbidly obese prior to their initial surgery and up to 35% of patients who were super obese have gained back more than 50% of their excess weight after 10 years (3). Sometimes this is the result of internal issues that require surgical revision while other times inappropriate diet or exercise is the culprit.
Gastric bypass revision surgery can carry risks just like your initial surgery, so it is important that you follow your surgeon’s orders exactly to avoid a second surgery if possible.
To this end, your surgeon will want to rule out diet or exercise problems before moving forward with another procedure and will likely take the following two steps (4):
- Rule out diet as the cause of insufficient weight loss or weight regain
- Work with your dietitian to very carefully track what you eat using a handwritten or online free diet journal.
- Work with your psychologist to determine whether any emotional issues could be causing your diet or exercise goals to veer off-track.
- Rule out exercise as the cause
- Your dietitian can use a special device called an indirect calorimeter (see video below) to test your basal metabolic rate (BMR), which is the amount of energy your body burns when you are resting.
Patients with an extremely low BMR could have issues with weight loss even if pouch size and dietary habits are where they should be. Your base metabolic rate can be increased if you add more lean body mass (muscle), so if low BMR is a problem your surgeon will most likely have you work with a personal trainer to properly adjust your exercise after gastric bypass surgery.
- Your dietitian can use a special device called an indirect calorimeter (see video below) to test your basal metabolic rate (BMR), which is the amount of energy your body burns when you are resting.
After diet and exercise problems are ruled out, your surgeon will want to check your stomach pouch size and the opening between your stomach and your small intestines (also called your “stoma”). If either is too large (or has stretched), it may be the cause of your post-surgery weight loss problems (5).
Your surgeon has a few ways to check this:
- Upper Gastrointestinal Tract Radiography (also called an “upper GI”) – Your surgeon will have you drink a special colored dye while taking an x-ray in order to see your digestive tract “in motion”.
- Endoscopy – After applying a numbing spray and/or medication, the surgeon will pass a tube with a camera through your mouth, down your esophagus and into your stomach to directly evaluate the size of your pouch and stoma.
- Eating test – Your surgeon will measure the amount of food you can eat before feeling full.
In addition to determining whether your pouch and stoma size are an issue, the upper GI and endoscopy can detect issues such as staple line problems, gastrogastric fistula, esophageal abnormalities and Roux limb abnormalities (6). Your surgeon will also confirm that you have no underlying medical issues that might prevent you from having a revision procedure, such as severe kidney problems.
If stomach stretching or stoma enlargement is identified, a revision surgery may be your only option to halt or reverse the weight regain.
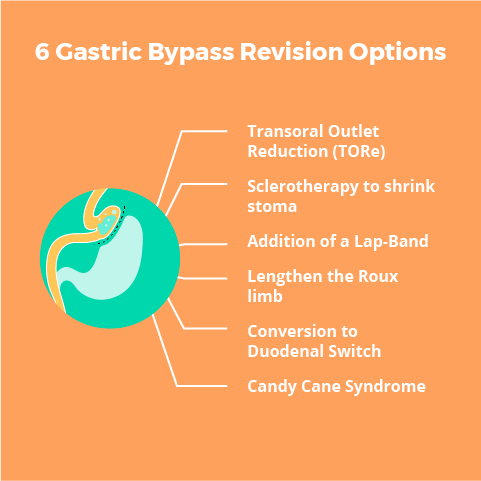
6 Gastric Bypass Revision Options
SECTION SUMMARY:
- Transoral Outlet Reduction (TORe)
- Sclerotherapy to shrink stoma
- Addition of a Lap-Band
- Lengthen the Roux limb
- Conversion to Duodenal Switch
- Candy Cane Syndrome
What about converting to Gastric Sleeve?
While “converting” from a gastric bypass to a gastric sleeve is technically possible, it is a complicated procedure that is not performed frequently.
Click here for more information.
In order to surgically facilitate weight loss, your surgeon will likely choose one of six ways to reduce your pouch and/or stoma size back to what it was (or what it should have been) after your initial procedure.
A reduced pouch size will cause your stomach to hold less, making you feel full sooner. A reduced stoma size will cause your stomach to drain more slowly, prolonging your feelings of fullness.
Sure that your original surgeon is right for the job?
Before getting into the six types of gastric bypass revision procedures, consider whether your original surgeon is right for the job.
If you took the proper steps towards finding, evaluating, interviewing and choosing your original weight loss surgeon, if the costs were right AND if you felt good about your experience, stick with your original team.
If you didn’t interview multiple surgeons or if something "just felt off" with your original team, it may be a good idea to interview another qualified surgeon to compare their abilities, team, services and cost.
The six most common gastric bypass revision procedures include:
1. Transoral Outlet Reduction (TORe)
The Transoral Outlet Reduction (TORe) is a procedure that addresses weight regain after gastric bypass. The goal is to reduce the size of the gastric pouch. The smaller the gastric pouch, the less food patients need to eat to feel full.
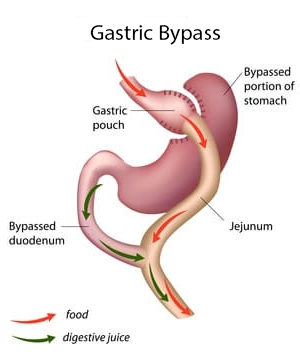
After gastric bypass, the gastric pouch can enlarge naturally or as a result of overeating. Using the TORe technique, surgeons are able to suture the enlarged gastric pouch to make it smaller. This delays food processing and keeps patients feeling full for a longer period of time.
This procedure is proven to contribute to weight loss after gastric bypass weight regain (7). Some patients report feeling as if they’d had a second gastric bypass. Practitioners report this is a low risk procedure with risks equivalent to that of a standard endoscopy.
Prior to the procedure, patients will fast overnight. The procedure can take anywhere from 30 to 90 minutes and patients return home that day. Return-to-work takes anywhere from 1 to 3 days.
Payment for the TORe runs approximately $8,000 to $10,000. Insurance companies may cover this procedure, so ask your provider.
2. Shrink the stoma by injecting a sclerosant ("sclerotherapy")
Your surgeon may decide that injecting a sclerosant (sodium morrhuate) into the stoma (opening between the stomach and small intestine) is the best way to address the relatively common problem of stoma dilation.
The injections – which will most likely need to be done over the course of two or three procedures – attempts to create scarring that reduces the stoma’s size.
One study showed that 64% of patients lost at least 75% of their weight regain after their injections (8).The only complication that occurred was symptoms of stomal stenosis that required the stomach to be stretched back out with the use of a special balloon.
Another study revealed that out of 231 patients who underwent 575 sclerotherapy sessions (9):
- 12 months from the last sclerotherapy session, weight regain stabilized in 78% of the patients
- Patients who underwent two or three sclerotherapy sessions had much higher rates of weight regain stabilization than those who underwent a single session
- The average sclerotherapy patient lost 10 pounds in six months
- There were ‘high responders’ who lost an average of 26 pounds, which was 61% of the weight regain
- Those who had higher regain after bariatric surgery responded better to sclerotherapy
The procedure does carry a low risk of minor complications including:
- Bleeding (2.5% of patients)
- Abdominal pain (0.5%)
- Small ulcers (1%)
- Transient, self-limited diastolic blood pressure elevation (11%)
Due to the relatively high risk of blood pressure elevation, patients with cardiac risk factors should most likely stay away from this procedure.
Click here to contact a surgeon about your revision options.
3. Addition of adjustable gastric band (lap band surgery)
At least three studies have directly evaluated the effect of inserting an adjustable gastric band (lap band) following failed gastric bypass surgery:
- Study 1 included 11 patients who, on average, received gastric bypass surgery 5 ½ years earlier. Their mean body mass index dropped from 43.4 to 37.1 (additional excess weight loss of about 21%) (10).
- Study 2 evaluated 22 patients and saw a drop in excess weight of 47% after five years (11).
- Study 3 compiled seven studies with 94 total patients who experienced between 55.9% and 94.2% excess weight loss 12 to 42 months after the placement of the band. About one in five of these patients developed long-term complications that required another operation (12).
You should expect the procedure, costs, health benefits and potential complications to be similar to having lap band surgery as an initial procedure.
See our Adjustable Gastric Banding page for more information.
Click here to contact a surgeon about your revision options.
4. Lengthen the Roux limb
This procedure converts a proximal (conventional) Roux-en-Y gastric bypass to a distal Roux-en-Y gastric bypass. It is usually only considered when the patient has a very low base metabolic rate and continues with poor weight loss results despite an augmented exercise program.
While this conversion should be effective for weight loss, it will open you up to increased risks – far more than with any other procedures. For example, one study reported a 15% leak rate following revision surgery (13).
For this reason, this procedure is not a standard primary approach for weight loss surgery and is why many surgeons feel that it is inappropriate even for the failed gastric bypass patient.
Click here to contact a surgeon about your revision options.
5. Conversion to Duodenal Switch
Patients requiring gastric bypass revision surgery – especially patients who were super obese prior to gastric bypass surgery (50+ BMI) – may find a conversion to duodenal switch surgery to be the best option.
For example, one study evaluated 12 patients undergoing a conversion from Roux-en-Y gastric bypass to a duodenal switch. The patients had an average original BMI of 53.9, an average low BMI after gastric bypass of 31.6 and an average pre-conversion BMI of 40.7. About one year after revision surgery, their average BMI was 31 (63% excess weight lost) (14).
Click here to contact a surgeon about your revision options.
6. Candy Cane Syndrome
It is possible that a no-longer-functioning portion of the small intestine near the new junction of the stomach and small intestine will cause patients abdominal pain, nausea, and vomiting. Once identified, the “Candy Cane” (the non-functioning portion of the intestine) is laparoscopically removed, and in the vast majority of cases (94%), patients experience complete resolution of their symptoms (15).
Click here to contact a surgeon about your revision options.
Find a Gastric Bypass Revision Surgeon
SECTION SUMMARY:
- You can ask a local bariatric practice for a free insurance check or cost quote for your revisional surgery
- You should schedule a phone or in-person consultation (both often free), if you are interested in learning more about revisional weight loss surgery
- Search the Weight Loss Revision Surgeon directory below to find a weight loss surgeon by country and region
Search the Weight Loss Revision Surgeon directory below to find a weight loss surgeon by country and region: