Lap band problems range from annoyances to complete failure and removal of the band. Lap band surgery does have fewer serious complications than other bariatric surgery procedures, but the prevalence of minor complications should be an important consideration for prospective patients.
This page reviews the details, including…

Band Removal
Eventually Required in Up to Half of All Patients
Band Removal – Eventually Required in Up to Half of All Patients
At around 0.1%, lap band surgery has an extremely low mortality rate (death rate). The bad news is the alarming rate of lap band complications, which in one study was as high as 26%.
Fortunately, many of the complications are minor and are easily repaired, and the typical worst case is the removal of the band.
Unfortunately, lap band removal is eventually required in up to 50% of all lap band patients – most commonly because of inadequate weight loss.
Following are the gastric banding mortality and complication rates from 5 separate studies…
Studies Studies |
Study F Study F |
Study A Study A |
Study B Study B |
Study C Study C |
Study E Study E |
Studies # of gastric banding patients in study |
Study F 714 |
Study A 1,176 |
Study B 400 |
Study C 179 |
Study E 190 |
Studies Mortality & Complication Rates |
Study F Mortality – 0% Revisional procedure required – 50.4% (proximal enlargement (pouch dilation) -26%; band erosion-3.4%; port and tubing problems-21%). STUDY NOTE: “The need for revision decreased as the technique evolved, with 40% revision rate for proximal gastric enlargements in the first 10 years, reducing to 6.4% in the past 5 years. The revision group showed a similar weight loss to the overall group beyond 10 years.” |
Study A Mortality – 0.09% Major complications – 1% All complications – 2.6% |
Study B Mortality -0.25% All complications – 8.8% |
Study C Mortality -0.56% Early complications – 2.8% Late complications – 26% 4 Years – 82.1% |
Study E Mortality – 0% All complications – 10.5% |
Studies Year |
Study F 2012 |
Study A 2008 |
Study B 2007 |
Study C 2007 |
Study E 2004 |
Complete List of Complications
A to Z List of All Potential Complications
Complete List of Complications – A to Z List of All Potential Complications
READ THIS FIRST
Are you experiencing complications with your gastric band?
We highly recommend contacting your previous surgeon or a top lap band revision surgeon to discuss the issues as soon as possible.
If you have not yet had weight loss surgery and are concerned about potential lap band issues, remember that most surgeons offer free seminars and/or free one-on-one consultations that teach you about your options and their office’s specific results, which may vary widely from practice to practice.
Following is a complete list of potential lap band problems. We have also included the percentage of patients who experience each when the information is available (where you see a range of percentages, multiple studies were found with varying results) (1) (2) (3) (4) (5) (6).
Click one of the following to jump down to more information or scroll down the page to review the complete list…Real-World Patient Experiences
It’s one thing to read about the potential list and general risks of complications, but it’s quite another to hear first hand how they can affect your life.
- Band problems (1.1% – 18% of gastric banding patients)
- Band erosion (2.1% – 9.5%) – (also called “band migration”) occurs when the band actually grows into the stomach. The only treatment is permanent removal of the band. See our Lap Band Erosion page for more information.
- Band intolerance – some patients’ bodies just can’t handle the band. After all, the band is a foreign object in your body. Band intolerance includes vomiting excessively or feeling uncomfortable all of the time. Permanent removal of the band is required in these cases.
- Band leak (1.1% – 4.9%) – patients can usually tell if their gastric banding system has a leak if their feelings of restriction decrease over time (thus increasing hunger) without the doctor unfilling the port. To determine whether you have a leak, your doctor may inject colored fluid and take an X-Ray to see if any of the colored fluid is present (from a leak) outside of the gastric banding system. Surgery is usually required to repair it.
- Band slippage (2% – 18%) – occurs when the lower part of the stomach “slips” through the band, creating a bigger pouch above the band. Either removing fluid (from the lap band) or surgical repositioning is required to repair band slippage. Symptoms include vomiting and reflux, and it is diagnosed by drinking a dye and using X-Ray to observe it. The band placement technique used by the surgeon also makes a difference – between the perigastric technique (PGT) and the pars flaccida technique (PFT), the pars flaccida technique appears to have a much lower rate of slippage (up to 16% less often) (7) (8) (9).
- Blood Clots (also called “thrombus”) – overweight people have a higher risk of developing blood clots during and after any kind of surgery. Blood thinners are often used to help prevent blood clots, along with special devices that squeeze the lower legs (“pneumatic compression devices”) to keep the blood flowing. Walking around periodically after surgery is also very effective. Symptoms of blood clots include swelling or pain in the legs and can be diagnosed by your doctor with an ultrasound. Blood clots are treated by a taking a prescribed blood thinner. If left untreated, clots can lead to a pulmonary embolism. Be sure to tell your doctor whether you or anyone in your family has a history of clotting. Smoking will increase your risk, so if you are a smoker it is recommended that you stop smoking as soon as possible before surgery – no later than two months out. For more information, see our Blood Clot Symptoms, Treatments & Prevention page.
- Bowel Function Changes – bowel function after lap band surgery may change, including…
- Constipation– usually corrected by increasing the amount of water you are drinking and by taking fiber supplements such as Fiber-Stat’s liquid fiber supplement.
- Difficulty swallowing (also called “dysphagia”) – caused by eating too quickly, too much or not chewing food enough and can usually be fixed by avoiding these habits.
- Bowel perforations (0.5% – 3.1%) occur when the bowel is punctured during surgery. Perforations are often caught and repaired right away, but it may take hours or days for them to show up, after which surgical repair will be required.
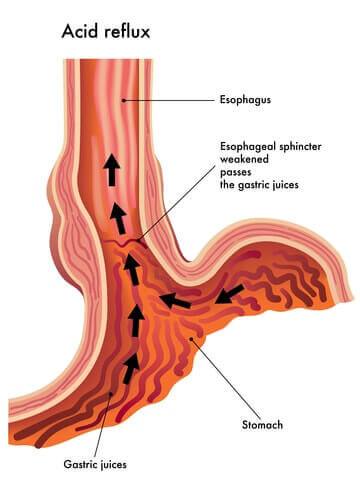
- Esophageal dilation (14%) ("dilated esophagus") is the enlarging of the esophagus and is usually the result of the band being too tight or being placed incorrectly. Most cases can be handled through deflation of the band under radiological control. GERD symptoms and vomiting are more frequent in patients who develop esophageal dilation.
Also see Achalasia.
- Food trapping occurs when food gets caught in one of the small openings in your digestive system. Food trapping is seen in 1 to 2% of gastric banding patients and is treated by deflating the band entirely until the food passes through.
- Gallstones – small stones of cholesterol formed in the gall bladder or bile passages. Gallstones can be created following rapid weight loss which leads to their development in as many as 1/3 of bariatric surgery patients. As a result, your surgeon may remove your gallbladder during surgery or prescribe bile salt supplements after surgery.
- Gastro-esophageal reflux disease (GERD) – a highly variable chronic condition that is characterized by periodic episodes of gastro-esophageal reflux usually accompanied by heartburn and that may result in histopathologic changes (change in the microscopic structure) of the esophagus. GERD often leads to esophagitis. While bariatric surgery can cause GERD, the condition is also improved for many following bariatric surgery.
Several at-home treatments are effective, including avoiding certain foods and drinks (alcohol, citrus juice, tomato-based food and chocolate), waiting 3 hours before lying down after a meal, eating smaller meals and elevating your head 8 inches when you lay down. If these don’t work, your doctor may recommend/prescribe antacids to be taken after meals and before going to bed, H2 blockers or even Proton Pump Inhibitors (PPI).
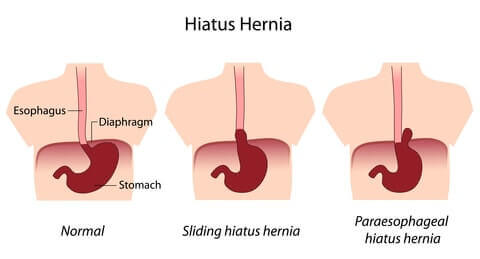
- Hiatal Hernia – a hernia in which an anatomical part (such as the stomach) protrudes through the esophageal hiatus (opening) of the diaphragm. Hiatal hernias can occur after restrictive procedures when food causes the smaller stomach to bulge and push through the diaphragm. It is not uncommon for an obese patient to already have a hiatal hernia before surgery. While a hiatal hernia can be a “contraindication” for surgery (reason that you may not be able to have the surgery), hiatal hernias can also be repaired during bariatric surgery.
- Indigestion (also called “dyspepsia”) – inability to digest or difficulty in digesting food; incomplete or imperfect digestion of food; a case or attack of indigestion marked especially by a burning sensation or discomfort in the upper abdomen. Treatment is usually as simple as changing your diet, such as avoiding greasy foods or only drinking liquids for a certain period of time. Alcohol, aspirin and other drugs are also causes. If diet changes don’t work, antacids and H2 blockers are sometimes prescribed.
- Intolerance to certain foods – With a changed stomach size or digestive system, there will be certain foods that you’ll need to avoid and certain diet habits you’ll need to maintain. See our Bariatric Diet section and Bariatric Eating page (how you eat vs what you eat) for more.
- Nausea and vomiting is one of the most common side effects of bariatric surgery and is experienced in up to 70% of patients. In one study, patients on average reported feeling nauseous 1.4 times per week and vomiting about once per week after gastric banding. Following the doctor’s orders regarding your bariatric diet will typically fix or improve the problem. While in the hospital, receiving a larger amount of IV fluids at a faster rate may make you less likely to feel nauseous or vomit.
- Pneumonia – a disease of the lungs that is characterized especially by inflammation and consolidation of lung tissue followed by resolution, is accompanied by fever, chills, cough, and difficulty in breathing, and is caused chiefly by infection. Obese patients are more likely to develop pneumonia post-surgery, so it is important that patients begin deep breathing and coughing exercises to prevent it. These exercises are much easier after laparoscopic surgery than after open surgery. Should pneumonia develop, it can be treated with antibiotics.
- Port problems (20.5% or about 1 in 5 gastric banding patients), including…
- Port flip/inversion or dislodgement (10.3%) occurs when the lap band port (where fluids are taken out or added to the band) “flips over”. This is typically not a serious problem and a quick procedure can turn it back over.
- Port Leak (1.1% – 4.9%) – as with a band leak, patients can usually tell if their gastric banding system has a leak if their feelings of restriction decreases over time (thus increasing hunger) without the doctor unfilling the port. To determine if you have a leak, your doctor may inject colored fluid and take an X-Ray to see if any of the colored fluid is present (from a leak) outside of the gastric banding system. Surgery is usually required to repair it.
- Port or band infection (1.5% – 5.3%) – if port or band infection occurs, it is usually healed with antibiotics, but removal of the band or port may be necessary.
- Port dislocation (6.9%) – similar to a port flip, a port dislocation means that your port has moved from its original location. It can be fixed with a simple operation under local anesthesia.
- Pouch dilation (6.3% – 16.9%) refers to the enlarging of the stomach pouch above the band. It may be fixed by removing fluid from the band, but surgery is sometimes required. Good outcomes can be expected after rebanding in properly assessed patients with slippage and pouch dilation.
While reviewing the above potential lap band problems and lap band complications, did you notice the number of complications that sometimes require reoperation? The percentage of patients requiring reoperation is extremely high… up to 50% of all patients require lap band removal.
“The percentage of patients requiring reoperation is extremely high, ranging from 11% to 37%.”
Fortunately, many of the reoperations are able to fix the problem by either repairing the gastric banding system or converting to one of several other bariatric surgery procedures.
See our Bariatric Surgery Complications page for a procedure by procedure comparison of complications along with what you need to do to minimize your risks. Our Lap Band vs Gastric Bypass page provides a more specific comparison between the two most popular bariatric surgery procedures.
Health Risks of Obesity Vs. Risks of Weight Loss Surgery
When deciding whether the risks of complications and mortality are “worth it”, it is a good idea to evaluate the risks of not having surgery. See our Life after Weight Loss Surgery, Obesity Health Problems and Cause and Effect of Obesity pages for more on this.
Lap Band Failure
Due to Poor Weight Loss or Complications
Lap Band Failure – Due to Poor Weight Loss or Complications
Still have questions or concerns about this page’s topic?
Our weight loss surgery community will be happy to share their experiences and advice.
Click here to post your question
…or…
There are 2 lap band problems that cause the surgery to be classified as a failure:
- Unsuccessful weight loss – “unsuccessful” carries a different definition with each surgeon, but in general a procedure is considered to be a failure if you lose 25 to 30% or less of your excess weight (in other words, if you’re 100 pounds overweight that would mean you lost 25 to 30 pounds or less).
- Complication(s) requiring the removal of the band.
Our Lap Band Surgery Failure page will take you through the details.
Help & Support
Patient Experiences, Ask the Expert
Help & Support*
Ask the Expert & Patient Experiences*
We would love to hear your experiences with Lap-band problems and complications. Your insights are invaluable to making sure other people have the tools to meet their goals.
We would also be happy to answer any questions you may have about Lap-band problems and complications.
Please use the form below to share your experience or ask a question.
Questions From Other Visitors*
Click below to see contributions from other visitors to this page.


