There are 7 types of weight loss surgery available, including:
- Gastric Sleeve – 50+% excess weight loss; permanent; feel less hungry & full sooner while eating
- Gastric Bypass – 50+% excess weight loss; permanent; feel full sooner while eating & absorb fewer minerals
- Duodenal Switch – 50+% excess weight loss; permanent; feel less hungry & full sooner while eating, absorb fewer calories and minerals
- Lap-Band – 50+% excess weight loss; reversible; feel full sooner while eating
- Gastric Balloon – under 30% excess weight loss; temporary; feel full sooner while eating
- vBloc Therapy – under 30% excess weight loss; reversible; feel full between meels & less hungry while eating
- AspireAssist – under 30% excess weight loss; reversible; drain a portion of stomach contents after eating
There is no “one size fits all” procedure, so this page will help you determine which ones best fit your goals.

Weight Loss
Ranges from Part to Most of Your Excess Weight
Weight Loss: Ranges from Part to Most of Your Excess Weight
Most Weight Loss
Winner: Duodenal Switch
Runners Up: (Tie) Gastric Sleeve & Gastric Bypass
Patients lose weight quickly after most procedures, with the low point coming 12 to 18 months after the procedure.
The duodenal switch (DS), gastric sleeve, and gastric bypass are very close in terms of their average low point, but the DS pulls ahead over the long-term as it results in less weight regain over time.
Excess Weight Loss by Procedure
The following graph and chart compare weight loss over time for each procedure:
Gastric Sleeve Gastric Sleeve |
Gastric Bypass Gastric Bypass |
Gastric Balloon Gastric Balloon |
Duodenal Switch Duodenal Switch |
Lap-Band Lap-Band |
vBloc Therapy vBloc Therapy |
AspireAssist AspireAssist |
3 Months |
Gastric Sleeve 30% |
Gastric Bypass 30% |
Gastric Balloon 15% |
Duodenal Switch 30% |
Lap-Band 20% |
vBloc Therapy 10% |
AspireAssist 8% |
6 Months |
Gastric Sleeve 50% |
Gastric Bypass 50% |
Gastric Balloon 30% |
Duodenal Switch 45% |
Lap-Band 30% |
vBloc Therapy 20% |
AspireAssist 15% |
1 Year |
Gastric Sleeve 70% |
Gastric Bypass 65% |
Gastric Balloon varies (balloon removed after 6 mo) |
Duodenal Switch 65% |
Lap-Band 40% |
vBloc Therapy 25% |
AspireAssist 30% |
2 Years |
Gastric Sleeve 65% |
Gastric Bypass 60% |
Gastric Balloon varies (balloon removed after 6 mo) |
Duodenal Switch 70% |
Lap-Band 55% |
vBloc Therapy 25% |
AspireAssist y no data yet |
3 years |
Gastric Sleeve 60% |
Gastric Bypass 60% |
Gastric Balloon varies (balloon removed after 6 mo) |
Duodenal Switch 70% |
Lap-Band 55% |
vBloc Therapy 25% |
AspireAssist no data yet |
5 years |
Gastric Sleeve 55.% |
Gastric Bypass 60% |
Gastric Balloon varies (balloon removed after 6 mo) |
Duodenal Switch 70% |
Lap-Band 55% |
vBloc Therapy 25% |
AspireAssist no data yet |
References: (1) (2) (3) (4) (5) (6) (7) (8) (9) (10) (11) (12) (13) (14) (15) (16) (17) (18) (19) (20) (21) (22) (23) (24) (25) (26) (27) (28) (29) (30)
Health Benefits
Diabetes, Cardiac, Asthma, Joints, Many Others
Health Benefits Diabetes, Cardiac, Asthma, Joints, Many Others
Best Health Improvement
Winner: Duodenal Switch
Runners Up: (Tie) Gastric Sleeve & Gastric Bypass
The duodenal switch (DS) seems to deserve more attention than it has gotten as it is the clear front-runner in terms of health improvement. In fact, DS surgery is even being performed on non-morbidly obese patients to treat metabolic syndrome and diabetes (1).
It works so well because it combines the restriction of gastric sleeve, making patients feel full sooner after eating, with its own brand of malabsorption to limit the number of calories that the body can absorb.
Despite its effectiveness, most surgeons tend to only consider it for super-obese patients (BMI of 50 or greater) because:
- It is more difficult to perform
- It takes longer to perform
- It requires much more diligent follow up for both surgeons and patients due to the the level of malabsorption that it causes
While not as good as the DS, gastric sleeve and gastric bypass have extremely impressive health improvement stats as well.
The following table compares available studies for all procedures and conditions:
Co-morbidity Co-morbidity |
Dyslipidemia hypercholesterolemia Dyslipidemia hypercholesterolemia |
Diabetes Diabetes |
Hyperlipidemia (high levels of fat in the blood, high cholesterol) Hyperlipidemia (high levels of fat in the blood, high cholesterol) |
High Blood Pressure (hypertension) High Blood Pressure (hypertension) |
Joint/Bone Disease (osteoarthropathy) Joint/Bone Disease (osteoarthropathy) |
Depression Depression |
Migraines Migraines |
Pseudotumor cerebri Pseudotumor cerebri |
Cardiovascular Disease Cardiovascular Disease |
Venous Stasis Disease Venous Stasis Disease |
Gastroesophageal Reflux Disease (GERD) Gastroesophageal Reflux Disease (GERD) |
Non-Alcoholic Fatty Liver Disease Non-Alcoholic Fatty Liver Disease |
Mortality Reduction/ Life Expectancy (5 year mortality) Mortality Reduction/ Life Expectancy (5 year mortality) |
Quality of Life Improvements Quality of Life Improvements |
Metabolic Syndrome Metabolic Syndrome |
Polycystic Ovarian Syndrome Polycystic Ovarian Syndrome |
Pregnancy Pregnancy |
Asthma Asthma |
Obstructive Sleep Apnea Obstructive Sleep Apnea |
Stress Urinary Incontinence Stress Urinary Incontinence |
Co-morbidity Gastric Balloon % Improved /Resolved |
Dyslipidemia hypercholesterolemia 10% |
Diabetes 33% |
Hyperlipidemia (high levels of fat in the blood, high cholesterol) 34% |
High Blood Pressure (hypertension) 45% |
Joint/Bone Disease (osteoarthropathy) 48% |
Depression |
Migraines |
Pseudotumor cerebri |
Cardiovascular Disease |
Venous Stasis Disease |
Gastroesophageal Reflux Disease (GERD) |
Non-Alcoholic Fatty Liver Disease |
Mortality Reduction/ Life Expectancy (5 year mortality) |
Quality of Life Improvements |
Metabolic Syndrome |
Polycystic Ovarian Syndrome |
Pregnancy |
Asthma |
Obstructive Sleep Apnea |
Stress Urinary Incontinence |
Co-morbidity Gastric Sleeve % Improved /Resolved |
Dyslipidemia hypercholesterolemia 64% |
Diabetes 55% |
Hyperlipidemia (high levels of fat in the blood, high cholesterol) 35% |
High Blood Pressure (hypertension) 68% |
Joint/Bone Disease (osteoarthropathy) 46% |
Depression Most |
Migraines 40% |
Pseudotumor cerebri n/a |
Cardiovascular Disease 100% |
Venous Stasis Disease 95% |
Gastroesophageal Reflux Disease (GERD) 50% |
Non-Alcoholic Fatty Liver Disease n/a |
Mortality Reduction/Life Expectancy (5 year mortality) 89% |
Quality of Life Improvements 93% |
Metabolic Syndrome 62% |
Polycystic Ovarian Syndrome Most |
Pregnancy Most |
Asthma 90% |
Obstructive Sleep Apnea 62% |
Stress Urinary Incontinence 90% |
Co-morbidity Bypass % Improved /Resolved |
Dyslipidemia hypercholesterolemia 63% |
Diabetes 83% |
Hyperlipidemia (high levels of fat in the blood, high cholesterol) 73% |
High Blood Pressure (hypertension) 69% |
Joint/Bone Disease (osteoarthropathy) 43% |
Depression Most |
Migraines 57% |
Pseudotumor cerebri 96% |
Cardiovascular Disease 79% |
Venous Stasis Disease 95% |
Gastroesophageal Reflux Disease (GERD) 80% |
Non-Alcoholic Fatty Liver Disease 90% |
Mortality Reduction/Life Expectancy (5 year mortality) 89% |
Quality of Life Improvements 95% |
Metabolic Syndrome 80% |
Polycystic Ovarian Syndrome Most |
Pregnancy Most |
Asthma 80% |
Obstructive Sleep Apnea 98% |
Stress Urinary Incontinence 88% |
Co-morbidity DS % Improved /Resolved |
Dyslipidemia hypercholesterolemia 99%% |
Diabetes 92% |
Hyperlipidemia (high levels of fat in the blood, high cholesterol) 99% |
High Blood Pressure (hypertension) 83% |
Joint/Bone Disease (osteoarthropathy) 43% |
Depression Most |
Migraines Most |
Pseudotumor cerebri — |
Cardiovascular Disease 86% |
Venous Stasis Disease — |
Gastroesophageal Reflux Disease (GERD) 49% |
Non-Alcoholic Fatty Liver Disease 99% |
Mortality Reduction/Life Expectancy (5 year mortality) 89% |
Quality of Life Improvements 95% |
Metabolic Syndrome 99% |
Polycystic Ovarian Syndrome Most |
Pregnancy — |
Asthma 90% |
Obstructive Sleep Apnea 99% |
Stress Urinary Incontinence — |
Co-morbidity vBloc % Improved /Resolved |
Dyslipidemia hypercholesterolemia — |
Diabetes Moderate |
Hyperlipidemia (high levels of fat in the blood, high cholesterol) — |
High Blood Pressure (hypertension) — |
Joint/Bone Disease (osteoarthropathy) — |
Depression — |
Migraines — |
Pseudotumor cerebri — |
Cardiovascular Disease Moderate |
Venous Stasis Disease — |
Gastroesophageal Reflux Disease (GERD) — |
Non-Alcoholic Fatty Liver Disease — |
Mortality Reduction/Life Expectancy (5 year mortality) — |
Quality of Life Improvements — |
Metabolic Syndrome — |
Polycystic Ovarian Syndrome — |
Pregnancy — |
Asthma — |
Obstructive Sleep Apnea — |
Stress Urinary Incontinence — |
Co-morbidity Band % Improved /Resolved |
Dyslipidemia hypercholesterolemia 70% |
Diabetes 60% |
Hyperlipidemia (high levels of fat in the blood, high cholesterol) 23% |
High Blood Pressure (hypertension) 43% |
Joint/Bone Disease (osteoarthropathy) 81% |
Depression 57% |
Migraines Some |
Pseudotumor cerebri Most |
Cardiovascular Disease 73% |
Venous Stasis Disease — |
Gastroesophageal Reflux Disease (GERD) 87% |
Non-Alcoholic Fatty Liver Disease Most |
Mortality Reduction/Life Expectancy (5 year mortality) 89% |
Quality of Life Improvements Most |
Metabolic Syndrome 78% |
Polycystic Ovarian Syndrome 48% |
Pregnancy Most |
Asthma 82% |
Obstructive Sleep Apnea 85% |
Stress Urinary Incontinence 82% |
Co-morbidity AsipreAssist % Improved/ Resolved |
Dyslipidemia hypercholesterolemia |
Diabetes Possible improvement |
Hyperlipidemia (high levels of fat in the blood, high cholesterol) Possible improvement |
High Blood Pressure (hypertension) Possible improvement |
Joint/Bone Disease (osteoarthropathy) |
Depression |
Migraines |
Pseudotumor cerebri |
Cardiovascular Disease |
Venous Stasis Disease |
Gastroesophageal Reflux Disease (GERD) |
Non-Alcoholic Fatty Liver Disease |
Mortality Reduction/Life Expectancy (5 year mortality) |
Quality of Life Improvements |
Metabolic Syndrome |
Polycystic Ovarian Syndrome |
Pregnancy |
Asthma |
Obstructive Sleep Apnea |
Stress Urinary Incontinence |
Qualify
Minimum Body Mass Index = 30
Qualify: Minimum Body Mass Index = 30
Easiest to Qualify
Winner: No Clear Winner
In order to qualify for any type of weight loss surgery, your body mass index (BMI) must fall within a certain range.
While gastric balloon is the only procedure to allow BMI’s between 30 and 35, it is also the only procedure to not allow BMI’s over 40.
vBloc Therapy also has a limited range of 35 to 45.
The rest of the procedures have the same qualification requirements:
- Body mass index above 40 or
- Body mass index between 35 and 40 as long as you have a serious obesity-related health problem (“comorbidity”) such as diabetes, asthma, hypertension, joint problems, sleep apnea, or one of many others.
Use the BMI Calculator below to determine your body mass index.
Your Weight Classification:
Below 18.5
Underweight
Your Health Risk:HighYou are considered to be underweight and should take physician-approved steps to gain weight.
18.5 – 24.9
Healthy Weight
Your Health Risk:Low25.0 – 29.9
Overweight
Your Health Risk:MODERATEYour risk increases to “High” if two or more of the following apply to you:
- You smoke cigarettes
- Family history of premature heart disease
- High blood glucose (blood sugar)
- High blood pressure (hypertension)
- Low HDL-cholesterol
(“good” cholesterol) - High LDL-cholesterol
(“bad” cholesterol) - High triglycerides
Your risk of health issues are even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
30.0 – 34.9
Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for gastric balloon surgery if you also have poorly controlled type 2 diabetes, have a higher risk of cardiovascular disease, or suffer from another weight-related health issue.
Talk with a surgeon to confirm that you qualify.
Learn Your Options35.0 – 39.9
Severely Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for any type of weight loss surgery if you also have one or more obesity-related health problems.
Talk with a surgeon to confirm that you qualify.
Learn Your Options40.0 – 49.9
Morbidly Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for any type of weight loss surgery, although gastric balloon is generally not approved for BMI’s over 40.
Your BMI indicates that you may be a good candidate for any type of weight loss surgery other than gastric balloon or vBloc Therapy.
Talk with a surgeon to confirm that you qualify.
Learn Your Options50 or Higher
Super Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for any type of weight loss surgery other than gastric balloon or vBloc Therapy.
Talk with a surgeon to confirm that you qualify.
Learn Your Options
Your Weight Classification:
Below 18.5
Underweight
Your Health Risk:HighYou are considered to be underweight and should take physician-approved steps to gain weight.
18.5 – 24.9
Healthy Weight
Your Health Risk:Low25.0 – 29.9
Overweight
Your Health Risk:MODERATEYour risk increases to “High” if two or more of the following apply to you:
- You smoke cigarettes
- Family history of premature heart disease
- High blood glucose (blood sugar)
- High blood pressure (hypertension)
- Low HDL-cholesterol
(“good” cholesterol) - High LDL-cholesterol
(“bad” cholesterol) - High triglycerides
Your risk of health issues are even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
30.0 – 34.9
Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for gastric balloon surgery if you also have poorly controlled type 2 diabetes, have a higher risk of cardiovascular disease, or suffer from another weight-related health issue.
Talk with a surgeon to confirm that you qualify.
Learn Your Options35.0 – 39.9
Severely Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for any type of weight loss surgery if you also have one or more obesity-related health problems.
Talk with a surgeon to confirm that you qualify.
Learn Your Options40.0 – 49.9
Morbidly Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for any type of weight loss surgery, although gastric balloon is generally not approved for BMI’s over 40.
Your BMI indicates that you may be a good candidate for any type of weight loss surgery other than gastric balloon or vBloc Therapy.
Talk with a surgeon to confirm that you qualify.
Learn Your Options50 or Higher
Super Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for any type of weight loss surgery other than gastric balloon or vBloc Therapy.
Talk with a surgeon to confirm that you qualify.
Learn Your Options
Cost
$8,150 – $27,000 Range, Financing Available for All
Cost: $8,150 – $27,000 Range, Financing Available for All
Low-Cost Procedure (Without Insurance)
Winner: Gastric Balloon (but long-term costs likely higher than more expensive procedures)
Runners Up: Lap Band (but long-term costs likely higher than more expensive procedures)
Low-Cost Procedure (With Insurance)
Winner: 4-Way Tie – Gastric Sleeve, Gastric Bypass, Duodenal Switch, & Lap-Band
Runners Up: Gastric Balloon
The cost of surgery should not dictate which procedure you have. Through research and consultation with your surgeon, you should move forward with the procedure that is most likely to work for you.
Still, if you don’t have insurance that covers bariatric surgery, it’s important to know what you’re up against financially.
*There are a few key caveats to the cost information and winners above:
- The above costs are averages. Actual costs vary widely depending on the region, hospital, and surgeon.
- These costs are not necessarily all inclusive.Talk with your surgeon or hospital for a more specific quote.
- Long-term costs will probably be much lower for the more expensive procedures. Even though they are not declared “Low-Cost Winners” in this section, the more expensive procedures tend to do a much better job at improving or resolving obesity-related health problems which will save you more money over the long-term. More on this in the “Cost of Not Having Surgery” sub-section below.
Financing
Regardless of which procedure you choose, financing is available to many patients to help make surgery more affordable.
Please visit our Financing weight loss surgery page for all the possible ways to finance your surgery.
Cost of Not Having Surgery vs. Cost of Weight Loss Surgery
Even if you’re paying out of pocket, the cost of any procedure is far less than the long-term costs of obesity-related health problems for morbidly obese people who don’t have surgery.
On average, weight loss surgery patients pay off their entire surgery and start getting ahead financially after only 2 years (2).
To illustrate: One study found that bariatric patients pay as much as $900 less per month as soon as 13 months after surgery than similar people who didn’t have surgery (3). Starting in month 13, that’s almost $11,000 saved per year in total medical costs.
Fewer prescription drugs alone have been found to save patients $3,000 or more per year (4).
Insurance
4 of 7 Procedures Currently Covered
Insurance: 4 of 7 Procedures Currently Covered
Insurance Coverage
Winner: (4-Way Tie) Sleeve, Bypass, Band, & Duodenal Switch
For insurance policies that include weight loss surgery, four procedures are currently covered:
- Gastric sleeve surgery
- Gastric bypass surgery
- Duodenal switch surgery (biliopancreatic diversion with duodenal switch)
- Gastric banding (Lap-Band surgery)
The weight loss surgery insurance approval process can take anywhere from 1 to 12 months, depending on your insurance company and your situation.
Following are the typical steps:
- Confirm with your doctor that your body mass index and health conditions fall within one of the two qualification requirements:
- BMI over 40 –OR–
- BMI over 35 with one or more of the following:
- Clinically significant obstructive sleep apnea
- Coronary heart disease
- Medically refractory hypertension
- Type 2 diabetes mellitus
- Other obesity-related health issues
- Complete 3 to 7 consecutive months of a medically supervised diet program, depending on your insurance company (can be coordinated by your bariatric surgeon).
- Schedule a consultation with your bariatric surgeon.
- Schedule a consultation with your primary care physician to obtain a medical clearance letter.
- Schedule a psychiatric evaluation to obtain a mental health clearance letter (usually coordinated by your bariatric surgeon).
- Schedule a nutritional evaluation from a Registered Dietitian (usually coordinated by your bariatric surgeon).
- Send all of the above documentation to your insurance company along with a detailed history of your obesity-related health problems, difficulties, and treatment attempts. The review process typically happens in under one month (usually coordinated by your bariatric surgeon).
- Insurance company sends approval or denial letter:
- If approved, your surgeon’s bariatric coordinator will contact you for scheduling.
- If denied, you can choose to appeal the denial.
Take the Easy Route – Your surgeon’s office will do most of this leg-work for you. They will be highly experienced in managing the process and may even have all of the required personnel on staff (e.g. registered dietitian, psychiatrist, bariatric coordinator, etc.).
Click here to access the weight loss surgeon directory to get started. Most offices will check your insurance for free to confirm coverage criteria.
For more information about weight loss surgery insurance, see our Bariatric Surgery Insurance Guide.
Procedure
7 Types Widely Performed
Procedure: 7 Types Widely Performed
Most Popular Procedure
Winner: Gastric Sleeve
Runners Up: Gastric Bypass
Procedure Fundamentals: Restriction, Malabsorption, & Vagal Nerve Stimulation
The established types of bariatric surgery work using one or more of the following techniques:
- Restrictive surgeries reduce the amount of food the stomach can hold. This makes you feel full much sooner after eating than you did before surgery. The established restrictive procedures include:
- Gastric sleeve
- Adjustable gastric banding (Lap-Band surgery)
- Intragastric balloon (gastric balloon)
- Malabsorptive surgeries rearrange and/or remove part your digestive system, which then limits the amount of calories, minerals, and/or fat soluble vitamins that your body can absorb. Treatments with a large malabsorptive component result in the most weight loss but may have higher complication rates. Malabsorptive surgeries include:
- Gastric bypass – mineral malabsorptive, not calorie malabsorptive
- Duodenal switch – mineral, calorie, and fat-soluble vitamin malabsorptive
- Vagal Nerve Blocking uses controlled electrical stimulation to block hunger signals sent from your stomach to your brain. The only FDA-approved device is:
- vBloc Therapy
- Aspiration uses gravity to empty a portion of your stomach’s contents through a system similar to a feeding tube. This prevents the food from being fully digested, leading to you losing weight. The only FDA-approve device is:
- AspireAssist
Experimental Procedures
Not included above are a few promising experimental procedures which can be reviewed on our Experimental Weight Loss Surgery page.
Rejected & Outdated Procedures
Two other procedures which are generally rejected by surgeons and/or outdated include:
Why They Work & How They’re Performed
This section reviews how each of the generally accepted procedures work and how they are performed, including videos for each. Click the procedures for more information:
Gastric Sleeve
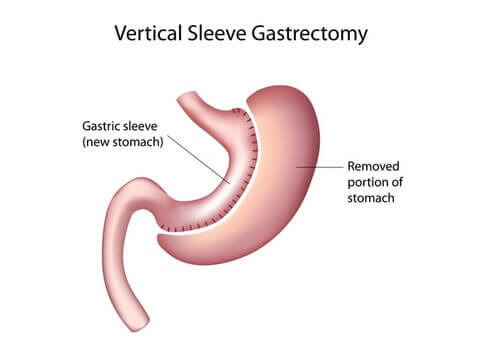
Why Gastric Sleeve Works
- Reduced stomach size makes the patient feel full sooner after eating
- Removed portion of the stomach means fewer hunger-causing hormones are secreted, causing patient to feel less hungry generally
How Gastric Sleeve Is Performed
Gastric sleeve surgery, also called the Vertical Sleeve Gastrectomy (VSG), is performed by removing a large portion of the stomach to create a long pouch that connects the esophagus to the small intestine. The pouch is stapled and the rest of the stomach is removed. Some surgeons take an additional step to reinforce the staple line, although whether that is effective is up for debate.
Gastric Bypass
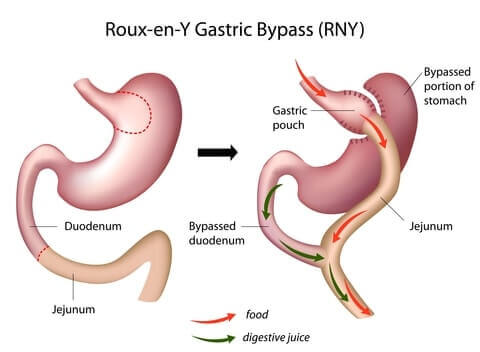
Why Gastric Bypass Works
- Reduced stomach size makes the patient feel full sooner after eating
- Rearranged intestines causes the body to absorb fewer minerals
- Dumping syndrome symptoms deter patients from eating unhealthy foods
How Gastric Bypass Is Performed
Gastric bypass, also called Roux-en-Y gastric bypass or RNY for short, is performed using the following steps:
- Cut and staple the top portion of the stomach to create a small pouch at the end of the esophagus
- Leave the remainder of the stomach attached to the top of the small intestines
- Go further down the small intestine, cut it, and attach it to the pouch
- Take the end of the small intestine that is still connected with the non-pouch portion of the stomach and attach it to the bottom of the “Roux limb.” This allows the digestive juices produced by the stomach to “meet up” with the food in the intestines.
Duodenal Switch (DS)
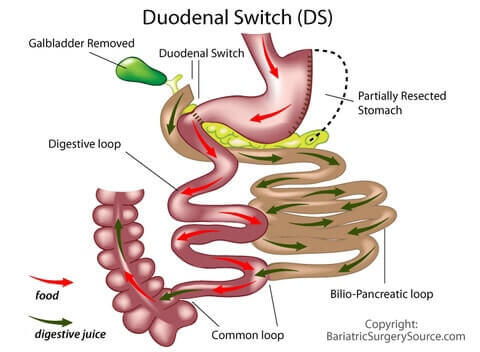
Why the Duodenal Switch Works
- Reduced stomach size makes the patient feel full sooner after eating
- Removed portion of the stomach means fewer hunger-causing hormones are secreted, causing patient to feel less hungry generally
- Rearranged intestines causes the body to absorb fewer calories and minerals
How the Duodenal Switch Is Performed
More formally known as the Biliopancreatic Diversion with Duodenal Switch, the DS surgeon starts with a gastric sleeve to reduce the stomach size, then rearranges the intestines to reduce the amount of calories the body can absorb.
Here are the steps:
- A large portion of the stomach is removed to create a banana-shaped pouch connecting the esophagus to the top of the small intestine (just like a gastric sleeve).
- The top of the small intestine is cut, but the surgeon leaves part of the duodenum, the top part of the small intestine where most chemical digestion occurs, attached to the stomach.
- The surgeon then cuts the small intestine several feet down. The part that is still attached to the large intestine (colon) is connected to the duodenum.
- The loose part of the small intestine (the part that wasn’t just attached to the stomach) is then attached to the small intestine so the digestive juices it creates can mix with the food coming from the stomach.
Gastric Bypass vs. Duodenal Switch: Clearing Up the Misconception
Both the DS and gastric bypass reduce the size of the stomach and rearrange the intestines. Both lead to substantial weight loss and health improvement.
So they’re kind of the same thing, right?
In fact, gastric bypass and the DS are just as different as any other two procedures. Here’s how they’re different:
- The DS stomach sleeve is much larger than the gastric bypass pouch
- The DS completely removes a large part of the stomach, whereas the gastric bypass leaves the separated part of the stomach attached to the small intestine
- Gastric bypass bypasses a much smaller portion of the small intestine, causing primarily mineral malabsorption. Calories are still largely absorbed after bypass. DS, on the other hand, bypasses a much longer portion of the small intestine, causing your body to absorb far fewer calories than after bypass. It also leads to much less absorption of minerals and fat soluble vitamins.
- Gastric bypass also bypasses the pylorus (the muscle that separates the stomach from the small intestine which is responsible for regulating how much food passes through the stomach and into the small intestine). The DS does not.
- Gastric bypass also bypasses the duodenum (the first portion of the small intestine where the digestive juices of the pancreas, liver, and gallbladder are secreted). The DS does not. Note that the duodenum is left in place after gastric bypass, but digestive juices secreted there “meet up” with the food much farther down the small intestines, greatly reducing their impact.
- The gallbladder is removed during DS surgery but is left in place after gastric bypass. The gallbladder stores digestive bile produced by the liver and releases it when you eat to help your body break down fats for absorption. Removing the gallbladder leads to even less calorie absorption for DS patients.
What do these differences mean to you?
- Gastric bypass has among the best weight loss and health improvement results among all procedures, but on average, DS is even better.
- DS has a higher risk of vitamin deficiency and requires more diligent follow up by surgeon and a stricter adherence to a vitamin regimen by the patient.
- Dumping syndrome is common for bypass patients and virtually non-existent for DS patients. Due to the much smaller stomach size and the bypassing of the pylorus and duodenum after gastric bypass, about 7 out of 10 gastric bypass patients experience dumping syndrome. Since the DS stomach sleeve is much larger and since the DS maintains the function of the pylorus and duodenum, DS patients do not experience dumping syndrome.
- DS is more complicated to perform. As a result, there are fewer experienced surgeons available to perform it. With all else being equal, whether or not DS has a higher risk of complications is unclear. Available research does show a higher DS complication rate, but:
- DS is more commonly performed on heavier patients who have an inherently higher risk of complications
- The more experienced the surgeon, the lower the risk of complications. Since the DS is much less common, surgeons often do not have as much experience performing it, leading to higher complication rates.
Is Dumping Syndrome Always a Bad Thing?

For about 95% of patients experiencing dumping syndrome, symptoms are relatively minor (5). Symptoms may include weakness, dizziness, flushing and warmth, nausea, and palpitation immediately or shortly after eating. They are caused by abnormally rapid emptying of the stomach, especially in individuals who have had part of the stomach removed.
While this sounds like a bad thing, many patients view it as a “blessing in disguise.” The symptoms of dumping syndrome are completely avoidable by eating a proper bariatric diet. Can you think of a more convincing way to keep you on track? In fact, some patients who do not suffer from dumping syndrome often comment that they wish they did, as “dumping” removes some of the choice involved in food selections. See our Dumping Syndrome page for more details.
Lap-Band
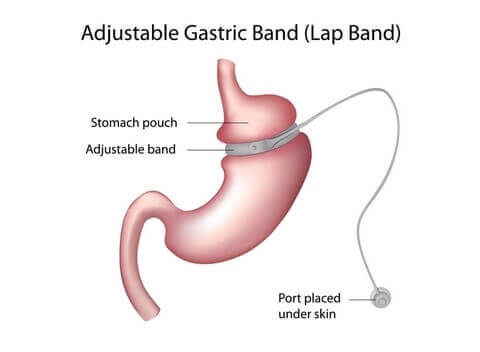
Why Lap-Band Surgery Works
- A band wraps around and squeezes a narrow section in the upper-middle part of the stomach. This creates a smaller stomach “section” above the band which fills up quicker after eating, causing the patient to feel full sooner and eat less.
How Lap-Band Surgery Is Performed
The Lap-Band, also called the gastric band or laparoscopic adjustable gastric band, has been used in Europe since the 90’s but wasn’t approved by the FDA in the States until 2001. It has since fallen out of favor in many practices due to its high long-term failure rate.
Apollo Endosurgery, Inc., the maker of the Lap-Band, insists that long-term failures are the result of patients not adhering to the strict follow up that is more typical among other procedures. They say they are reinventing their support process to improve Lap-Band’s reputation.
The Lap-Band surgery procedure involves the sewing of a silicone and Silastic band around the top of the stomach. A balloon around the inner surface of the band (imagine the inside of a bicycle tire) is connected to a tube that leads to a half-dollar-sized port above the abdominal muscles but below the skin.
During follow up visits, your doctor will add or remove saline solution (salt water) to make it tighter or looser. The tighter it is, the less hungry you feel and vice-versa.
vBloc Therapy
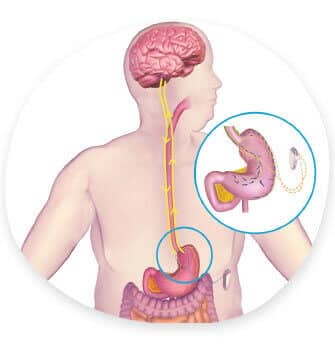
Why vBloc Therapy Works
- Implanted device periodically blocks the vagal nerve and prevents it from delivering hunger signals to the brain, making you feel full between meals and full sooner after smaller meals.
How vBloc Device Implantation Is Performed
Your surgeon will implant the vBloc Therapy device below your rib cage just under the skin. She will then attach the device to your vagal nerve, just above the stomach, via two leads (wires). The whole procedure usually takes between 60 and 90 minutes.
Gastric Balloon
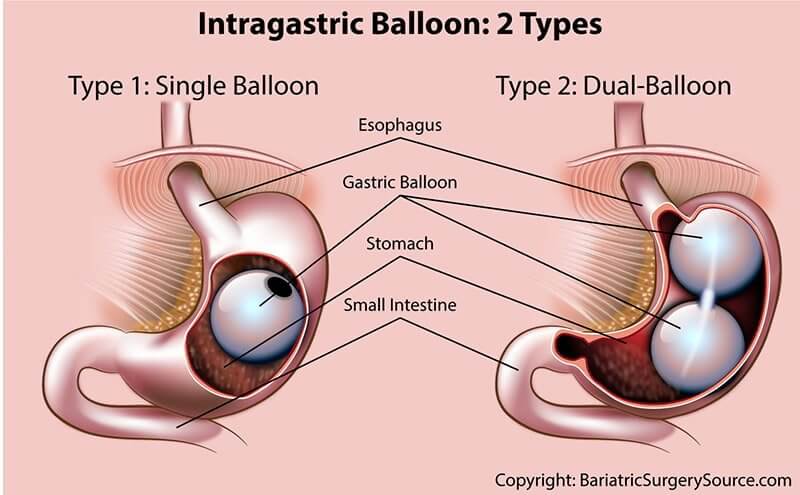
Why the Gastric Balloon Works
- An inflated balloon in the stomach leaves less room for food and causes patients to feel full sooner and eat less.
How the Gastric Balloon Is Inserted
The gastric balloon procedure is performed as follows:
- Surgeon numbs throat using a spray
- Patient may receive a sedative
- Plastic mouth guard is inserted in patient’s mouth for the scope to pass through
- Scope is passed through mouth and into stomach
- Scope is removed and balloon is passed into patient’s stomach
- Balloon is inflated with air or saline solution (depending on balloon type)
- Scope is passed into stomach again to confirm proper balloon positioning
Since it usually must be removed within 6 months, the balloon is only a temporary solution intended to “jump start” a long-term, medically-supervised diet and exercise program.
AspireAssist Device
Why the AspireAssist Works
- A tube similar to a feeding tube is inserted into the stomach and attached to a port on the outside of the abdomen. A device is then attached to this port and used to drain a portion of the stomach’s contents before digestion.
The AspireAssist Tube is inserted as follows:
- An endoscope is inserted in your mouth and passed through to your stomach.
- A small incision is made in your abdomen and a wire is passed through the incision into your stomach.
- The endoscope grabs the wire, and then both the endoscope and wire are pulled back out of your mouth.
- The “A-Tube” is then attached to the wire, and both are pulled back into your stomach and out the incision in your abdomen until the tip of the tube exits your incision.
- After your incision has healed you will need to go back to the doctor for a very quick procedure to attach your Skin-Port.
Recovery – In Hospital
6 Hours – 4 Days; Back to Work: 3 – 14 Days
Recovery – In Hospital: 6 Hours – 4 Days; Back to Work: 3 – 14 Days
Quickest Recovery
Winner: (Tie) vBloc Therapy, Gastric Balloon & AspireAssist
Runners Up: Lap-Band
The amount of time you’ll spend in the hospital and the recovery time depends on how “involved” your procedure is (how complicated the procedure is, whether part of the stomach is removed or digestive system rearranged, etc).
Less Involved Procedures
- Gastric balloon
- vBloc Therapy
- AspireAssist
The less involved procedures, including gastric balloon and vBloc Therapy, have the shortest hospital times (return home the same day as surgery) and recovery times (back to work in 3 to 4 days).
More Involved Procedures
- Lap-Band
- Gastric sleeve
- Gastric bypass
- Duodenal switch
The moderately involved procedure, Lap-Band, will require a 1 day hospital stay and will have you back to work in 2 weeks.
The most involved procedures, including gastric sleeve, gastric bypass, and duodenal switch, typically require 2 to 3 days in the hospital, although you should still be able to return to work within 2 weeks.
Recovery: What to Expect
For all procedures except gastric balloon and AspireAssist, here’s what to expect during your hospital stay and recovery:
- Wake Up: When you first awake after surgery, you’ll be sore and a little “out of it.” You’ll be on medication to control the pain.
- Move Around: Your surgeon will have you up and walking around as soon as possible after you wake up to reduce the risk of blood clots and jump-start your body’s healing process. Continue to walk as much as possible, increasing it a little each day.
- Get Released: Before releasing you, your surgical team will run a number of tests to ensure:
- You are able to drink enough to stay hydrated
- You can urinate normally after your catheter is removed
- You have adequate pain relief from your pain meds
- Look for Warning Signs: Warning signs vary by procedure. Call your surgeon immediately if you experience any of the following:
- Fever
- No improvement or worsening of pain
- Signs of incision infection (pus, swelling, heat, or redness)
- Difficulty swallowing
- Ongoing nausea or vomiting
- Transition Your Diet: Since you’ll be eating less, you may feel tired and lethargic until your body adjusts. For all procedures other than vBloc and gastric balloon, your smaller or constricted stomach will be sensitive, especially at first. You’ll be on a liquid diet for a couple of weeks before slowly transitioning back to solid foods (read more about this in the Diet & Life After section of this page).
- Ease Off Medications: Your surgeon will prescribe pain and digestion medication as needed and may adjust your pre-surgery medications until you’re fully healed. Follow their instructions to the letter.
- Return to Your “New Normal” Life: Avoid swimming or bathing until your incisions have fully healed. Many patients return to normal life and work within a couple of weeks, but plan for up to 4 to 6 weeks off to be on the safe side. Full exercise and heavy lifting typically resume within one to two months.
- Have Follow-Up Visits During First Year: Follow-ups with your surgeon’s team will happen about one week post-op, then around 4 weeks post-op, then every 3 or 4 months to ensure that everything is on track, including:
- Discuss weight loss
- Encourage regular exercise
- Obtain lab work and make necessary adjustments to medications and dietary supplements
- Understand diet and identify any potential eating disorders
- Determine whether any potential complications may be arising
- Monitor status of obesity-related health issues
- Involve your family physician to help evaluate progress and ensure a successful transition
- Transition to Semi-Annual or Yearly Follow-Up Visits: After you’ve reached your “low point” weight, your surgeon will probably still want to see you at least once per year (6). During those visits you may meet with several team members, including your surgeon, dietitian, and mental health care provider. They will probably request lab work to ensure that vitamin levels and other indicators are where they should be. If you experience any issues in between visits, don’t wait for your next visit… call your doctor right away.
Gastric balloon surgery recovery is unique in that it does not require any incisions. As a result, recovery is much faster than after the more involved procedure and generally focuses on diet changes:
- Day 1 – Clear Liquids Only
- Days 2 through 7 – Liquid Diet
- Days 7 through 14 – Pureed Food Diet
- Days 15+ – “New Normal” Diet – Restrictions include foods that may stick to your balloon, such as pasta. Sip water after you eat to rinse your balloon.
AspireAssist insertion recovery is unique because it is a relatively simple procedure requiring less time for recovery and does not necessarily require any long-term diet restrictions.
The procedure usually takes about 15 minutes and you should be able to return to your regular routine in about 3 days.
Because food will need to fit through the newly inserted tube your initial diet will be:
- Week One – pureed food or non-chunky soup
- Week Two – soft foods like bananas or pasta
- After Week Two – new healthy diet recommended by your surgeon/dietitian
Diet Changes
Ranges from Moderate to Significant
Diet Changes: Ranges from Moderate to Significant
Best Post-Op Diet
Winner: Depends on Patient’s Goals
The “best” long-term diet after weight loss surgery means different things to different people. For example, “best” could mean:
- Most weight loss, regardless of sacrifices
- Fewest long-term diet changes, even if less weight loss
- Anywhere in between
Unfortunately, you can’t have it all, so the following sections provide an overview of what to expect after each procedure.
Food & Drink: Varies by Procedure
Food & Drink: Varies by Procedure
The more involved procedures, including gastric sleeve, gastric bypass, duodenal switch, and Lap-Band, have very similar diet requirements before and after surgery. Gastric balloon, vBloc Therapy, and AspireAssist have their own guidelines.
The following sections compare each aspect of your diet after surgery.
Diet Stages & Timing By Procedure
Following is a general overview and timing of each stage before and after surgery:
Practice your post-surgery diet Practice your post-surgery diet |
High protein, low sugar, low carbs High protein, low sugar, low carbs |
Stop or change some medications Stop or change some medications |
Clear liquids only Clear liquids only |
Nothing to eat or drink Nothing to eat or drink |
Sugar-free clear liquids only Sugar-free clear liquids only |
Add thicker drinks & smooth foods Add thicker drinks & smooth foods |
Slowly test pureed foods & soft solid foods Slowly test pureed foods & soft solid foods |
Slowly test solid foods Slowly test solid foods |
Sleeve, Bypass, DS, Band |
Practice your post-surgery diet 2+ Weeks Before |
High protein, low sugar, low carbs 2 Weeks Before |
Stop or change some medications 1 Week Before |
Clear liquids only 2 Days Before |
Nothing to eat or drink Midnight Before Surgery |
Sugar-free clear liquids only In Hospital to 7 Days After Surgery (Varies by Surgeon) |
Add thicker drinks & smooth foods Day 1 to Week 2 After Surgery (Varies by Surgeon) |
Slowly test pureed foods & soft solid foods Day 2 to Week 3 After Surgery (Varies by Surgeon) |
Slowly test solid foods Day 3 to Weeks 4+ After Surgery (Varies by Surgeon) |
vBloc |
Practice your post-surgery diet — |
High protein, low sugar, low carbs — |
Stop or change some medications — |
Clear liquids only — |
Nothing to eat or drink Midnight Before Until After Surgery |
Sugar-free clear liquids only Until After Surgery |
Add thicker drinks & smooth foods — |
Slowly test pureed foods & soft solid foods — |
Slowly test solid foods — |
Balloon |
Practice your post-surgery diet 2+ Weeks Before |
High protein, low sugar, low carbs — |
Stop or change some medications — |
Clear liquids only — |
Nothing to eat or drink Midnight Before Until After Balloon Placement |
Sugar-free clear liquids only Until After Balloon Placement |
Add thicker drinks & smooth foods Day 2 through 7 |
Slowly test pureed foods & soft solid foods Day 6 through 14 |
Slowly test solid foods Weeks 3+ |
AspireAssist |
Practice your post-surgery diet — |
High protein, low sugar, low carbs — |
Stop or change some medications — |
Clear liquids only — |
Nothing to eat or drink Midnight Before Until After Tube Placement |
Sugar-free clear liquids only In Hospital to 7 Days After Surgery (Varies by Surgeon) |
Add thicker drinks & smooth foods — |
Slowly test pureed foods & soft solid foods Day 1 to Week 2 After Surgery (Varies by Surgeon) |
Slowly test solid foods After Week 2 |
Foods to Avoid By Procedure
For all procedures other than vBloc Therapy and the AspireAssist, your dietitian is likely to recommend the following:
- Test one food at a time to make sure you can tolerate it
- Eat proteins first, in solid form (e.g. not protein shakes)
- Eat healthy “whole” foods
- Avoid processed foods
- Avoid sugary foods or drinks
- Eat slowly and chew thoroughly
- No starchy foods like rice, bread, and pasta
- Avoid any food that is difficult to digest (may be able to tolerate over time), such as:
- Fibrous vegetables like broccoli, celery, and corn
- Nuts
- Seeds
- Skin of any meat
- Tough meats
- Avoid whole milk products
- Drink 64+ oz (2+ liters) of fluids spread throughout the day
- No drinking 30 minutes before or after meals (other than gastric balloon)
In addition to the above, following are procedure-specific foods to avoid:
- Gastric bypass
- Avoid foods that are likely to cause dumping, including sugar, unnecessary fat, or refined carbohydrates.
- Gastric balloon
- Avoid foods that may stick to your balloon and cause vomiting, such as pasta. To reduce risk of vomiting, drink liquids after eating to rinse your balloon.
Vitamins & Supplements
All Types of Bariatric Surgery
Since you will be eating less after any type of weight loss surgery, you will likely need to supplement your diet with:
- Daily multivitamin
- 1 to 2 per day, forever
- Chewable or liquid versions are best (instead of tablets)
- Take with food (except dairy) to maximize absorption
- At least 200% of the Recommended Dietary Allowance (RDA) of iron, folic acid, thiamine, copper, selenium and zinc
- Daily calcium supplement, in the form of calcium citrate
- Must be calcium citrate (NOT other forms of calcium)
- 1000-1500 mg. daily, forever
- Chewable and liquid versions are best (instead of tablets)
- Try to find one that includes Vitamin D
- Take 2 hours apart from Iron supplements (or Multivitamin that contains Iron) to maximize absorption
Gastric Sleeve, Gastric Bypass, Duodenal Switch, & Lap-Band Only
The more involved procedures, including the sleeve, bypass, DS, and band, may also require one or more of the following supplements, depending on your situation:
- Folate (folic acid)
- Iron
- Thiamin (Vitamin B1)
- Vitamin D
Gastric Bypass and Duodenal Switch Only
In addition to the above, Thiamin (Vitamin B1) supplementation is more likely to be required after gastric bypass and DS surgery given their higher levels of malabsorption than the other procedures.
Duodenal Switch Only
In addition to all of the above, since DS surgery is the only true malabsorptive procedure (malabsorption of calories, minerals, and fat-soluble vitamins vs only minerals after gastric bypass), DS patients also require daily fat-soluble vitamin supplements (including Vitamins A, D, E, and K).
This will typically include one additional tablet taken 3 times each day.
AspireAssist
As part of your follow up visits your surgeon will continue to monitor your nutrition levels. It is possible your surgeon will recommend you take additional vitamins if she determines you are not getting enough nutrients due to aspiration.
Exercise: Same for All Procedures
Exercise: Same for All Procedures
Following recovery, exercise should be the same for all procedures: 2.5 hours per week, spread out over 2 to 4 days. Keep in mind that patients who exercise regularly:
- Lose more weight
- Are more physically and mentally healthy
Learn more on our Exercise After Weight Loss Surgery page.
Your Brain: Less Hungry After Some Procedures, Careful About Food Addiction
Your Brain: Less Hungry After Some Procedures, Careful About Food Addiction
Reduced Hunger: Sleeve, DS, & vBloc Therapy
You may feel less hungry following the 2 procedures that completely remove a large portion of the stomach – gastric sleeve and duodenal switch.
When your stomach is empty, it secretes a hormone called ghrelin into your bloodstream which causes your brain to generate hunger impulses. After you eat, the amount of secreted ghrelin drops then slowly rises until your next meal. Since your stomach will be significantly smaller following these two procedures, the amount of ghrelin the stomach secretes – and your resulting feelings of hunger – may also go down.
vBloc Therapy is all about controlling hunger but goes about it differently. Instead of removing part of the stomach to control hormones, it uses an implanted device to block hunger signals altogether during certain parts of the day.
The other procedures leave the stomach in place and do not utilize a hunger-blocking device, so changes to hunger will remain largely unaffected.
Food Addiction
Regardless of which procedure you have, food addiction could be a problem.
Our bodies secrete certain hormones, like ghrelin mentioned above, that tell us when we’re hungry and full, but hyperpalatable food (like junk food) may be overriding those hormone signals by overstimulating our reward centers, much like our bodies and brains react to an addictive drug.
You may have a bona fide food addiction if your desire for food takes priority over other parts of your life that you acknowledge to be more important, such as personal health, family, friends, work, your appearance, or avoiding obesity related health issues like hypertension, sleep apnea, or diabetes.
If left unchecked, food addiction can lead to obesity. For weight loss surgery patients, if not addressed prior to surgery, it can also lead to weight regain.
To find out if you may be suffering from food addiction, take our Food Addiction Quiz.
Relationships After Weight Loss
Significant weight loss after any type of bariatric surgery can lead to big changes with everyone around you.
While many of those changes are positive, some can also be extremely challenging and unexpected.
See our Relationships After Weight Loss Surgery page for important changes to prepare for.
Downsides
Risk of Complications, Side Effects, & Weight Regain
Downsides: Risk of Complications, Side Effects, & Weight Regain
Fewest Risks & Side Effects
Winner: vBloc Therapy
Runners Up: (Tie) Gastric Balloon & Gastric Sleeve
Generally speaking, the types of bariatric surgery that result in more weight loss are often accompanied by higher risk and additional lifestyle changes.
The following chart highlights which complications are possible. Note that many complications listed below are associated with any type of surgery, bariatric or otherwise, and are relatively rare. For complications with procedure-specific research, we have included specific percentages.
Issue Issue |
Abdominal Discomfort Abdominal Discomfort |
Abdominal hernia Abdominal hernia |
Abscess Abscess |
Anemia Anemia |
Band Problems (band erosion, band infection, band intolerance, band leak, band slippage) Band Problems (band erosion, band infection, band intolerance, band leak, band slippage) |
Blood Clots Blood Clots |
Body Aches Body Aches |
Body Feeling Changes Body Feeling Changes |
Bowel Function Changes (diarrhea, constipation, foul-smelling bowel movements and flatulence, difficulty swallowing, gurgling noises) Bowel Function Changes (diarrhea, constipation, foul-smelling bowel movements and flatulence, difficulty swallowing, gurgling noises) |
Bowel Obstruction Bowel Obstruction |
Deep Vein Thrombosis Deep Vein Thrombosis |
Dehydration Dehydration |
Dental Problems Dental Problems |
Dumping Syndrome Dumping Syndrome |
Dyspepsia (Indigestion) Dyspepsia (Indigestion) |
Esophageal Dilation Esophageal Dilation |
Esophagitis Esophagitis |
Evisceration & Incisional Hernia Evisceration & Incisional Hernia |
Food Trapping Food Trapping |
Gallstones Gallstones |
Gastric Fistula Gastric Fistula |
Gastritis Gastritis |
Gastroesophageal Reflux Disease (GERD) Gastroesophageal Reflux Disease (GERD) |
Gastrointestinal Leaks Gastrointestinal Leaks |
General Anesthesia Complications General Anesthesia Complications |
Hair Loss Hair Loss |
Heart Attack Heart Attack |
Hemorrhage (Bleeding) Hemorrhage (Bleeding) |
Hiatal Hernia Hiatal Hernia |
Hypoglycemia Hypoglycemia |
Infection Infection |
Intolerance to Certain Foods Intolerance to Certain Foods |
Kidney Stones Kidney Stones |
Marginal Ulcers Marginal Ulcers |
Nausea, Vomiting and/or Stomach Cramps Nausea, Vomiting and/or Stomach Cramps |
Organ Injury During Surgery Organ Injury During Surgery |
Peritonitis Peritonitis |
Pneumonia Pneumonia |
Port Problems (port flip/ inversion or dislodgement, port leak, port infection, port dislocation) Port Problems (port flip/ inversion or dislodgement, port leak, port infection, port dislocation) |
Pouch Dilation Pouch Dilation |
Pulmonary Embolism Pulmonary Embolism |
Respiratory Failure Respiratory Failure |
Skin Changes (e.g. acne, dry skin, sagging skin, etc.) Skin Changes (e.g. acne, dry skin, sagging skin, etc.) |
Stenosis/Stricture Stenosis/Stricture |
Stoma Obstruction Stoma Obstruction |
Stroke Stroke |
Thrombophlebitis Thrombophlebitis |
Thrush (Yeast Infection) Thrush (Yeast Infection) |
Vitamin & Mineral Deficiency / Malnutrition / Malabsorption Vitamin & Mineral Deficiency / Malnutrition / Malabsorption |
Weight Regain Weight Regain |
Wound Reopening Wound Reopening |
Wound Sepsis Wound Sepsis |
Issue Complication or Side Effect |
Abdominal Discomfort Side Effect |
Abdominal hernia Complication |
Abscess Complication |
Anemia Side Effect |
Band Problems (band erosion, band infection, band intolerance, band leak, band slippage) Complication |
Blood Clots Complication |
Body Aches Side Effect |
Body Feeling Changes Side Effect |
Bowel Function Changes (diarrhea, constipation, foul-smelling bowel movements and flatulence, difficulty swallowing, gurgling noises) Side Effect |
Bowel Obstruction Complication |
Deep Vein Thrombosis Complication |
Dehydration Side Effect |
Dental Problems Side Effect |
Dumping Syndrome Side Effect |
Dyspepsia (Indigestion) Side Effect |
Esophageal Dilation Side Effect |
Esophagitis Side Effect |
Evisceration & Incisional Hernia Complication |
Food Trapping Side Effect |
Gallstones Side Effect |
Gastric Fistula Complication |
Gastritis Side Effect |
Gastroesophageal Reflux Disease (GERD) Side Effect |
Gastrointestinal Leaks Complication |
General Anesthesia Complications Complication |
Hair Loss Side Effect |
Heart Attack Complication |
Hemorrhage (Bleeding) Complication |
Hiatal Hernia Complication |
Hypoglycemia Complication |
Infection Complication |
Intolerance to Certain Foods Side Effect |
Kidney Stones Side Effect |
Marginal Ulcers Side Effect |
Nausea, Vomiting and/or Stomach Cramps Side Effect |
Organ Injury During Surgery Complication |
Peritonitis Complication |
Pneumonia Complication |
Port Problems (port flip/ inversion or dislodgement, port leak, port infection, port dislocation) Complication |
Pouch Dilation Complication |
Pulmonary Embolism Complication |
Respiratory Failure Complication |
Skin Changes (e.g. acne, dry skin, sagging skin, etc.) Side Effect |
Stenosis/Stricture Complication |
Stoma Obstruction Complication |
Stroke Complication |
Thrombophlebitis Complication |
Thrush (Yeast Infection) Side Effect |
Vitamin & Mineral Deficiency / Malnutrition / Malabsorption Side Effect |
Weight Regain Side Effect |
Wound Reopening Complication |
Wound Sepsis Complication |
Issue System |
Abdominal Discomfort Digestive |
Abdominal hernia Digestive |
Abscess integumentary (Skin) |
Anemia Circulatory |
Band Problems (band erosion, band infection, band intolerance, band leak, band slippage) Device |
Blood Clots Circulatory |
Body Aches Muscular |
Body Feeling Changes Central Nervous |
Bowel Function Changes (diarrhea, constipation, foul-smelling bowel movements and flatulence, difficulty swallowing, gurgling noises) Digestive |
Bowel Obstruction Digestive |
Deep Vein Thrombosis Circulatory |
Dehydration Full body |
Dental Problems Skeletal |
Dumping Syndrome Digestive |
Dyspepsia (Indigestion) Digestive |
Esophageal Dilation Digestive |
Esophagitis Digestive |
Evisceration & Incisional Hernia n/a |
Food Trapping Digestive |
Gallstones Digestive |
Gastric Fistula Digestive |
Gastritis Digestive |
Gastroesophageal Reflux Disease (GERD) Digestive |
Gastrointestinal Leaks Digestive |
General Anesthesia Complications Central Nervous |
Hair Loss integumentary (Skin) |
Heart Attack Circulatory |
Hemorrhage (Bleeding) Circulatory |
Hiatal Hernia Digestive |
Hypoglycemia Circulatory |
Infection Full body (Immune) |
Intolerance to Certain Foods Digestive |
Kidney Stones Digestive |
Marginal Ulcers Digestive |
Nausea, Vomiting and/or Stomach Cramps Digestive |
Organ Injury During Surgery Full body |
Peritonitis n/a |
Pneumonia respiratory |
Port Problems (port flip/ inversion or dislodgement, port leak, port infection, port dislocation) device |
Pouch Dilation Digestive |
Pulmonary Embolism respiratory |
Respiratory Failure respiratory |
Skin Changes (e.g. acne, dry skin, sagging skin, etc.) integumentary (Skin) |
Stenosis/Stricture Digestive |
Stoma Obstruction Digestive |
Stroke Central Nervous |
Thrombophlebitis Circulatory |
Thrush (Yeast Infection) integumentary (Skin) |
Vitamin & Mineral Deficiency / Malnutrition / Malabsorption Digestive |
Weight Regain Full body |
Wound Reopening integumentary (Skin) |
Wound Sepsis integumentary (Skin) |
Issue Sleeve |
Abdominal Discomfort — |
Abdominal hernia Yes |
Abscess Yes |
Anemia — |
Band Problems (band erosion, band infection, band intolerance, band leak, band slippage) — |
Blood Clots Yes |
Body Aches Yes |
Body Feeling Changes Yes |
Bowel Function Changes (diarrhea, constipation, foul-smelling bowel movements and flatulence, difficulty swallowing, gurgling noises) Yes |
Bowel Obstruction Yes |
Deep Vein Thrombosis Yes |
Dehydration Yes |
Dental Problems — |
Dumping Syndrome — |
Dyspepsia (Indigestion) Yes |
Esophageal Dilation Yes |
Esophagitis Yes |
Evisceration & Incisional Hernia Yes |
Food Trapping — |
Gallstones Up to 1/3 of bariatric patients |
Gastric Fistula Yes |
Gastritis Yes |
Gastroesophageal Reflux Disease (GERD) About 20% after 1 year; About 3% after three years |
Gastrointestinal Leaks About 2% of patients |
General Anesthesia Complications Yes |
Hair Loss Yes |
Heart Attack Yes |
Hemorrhage (Bleeding) About 1% of patients |
Hiatal Hernia Yes |
Hypoglycemia — |
Infection Yes |
Intolerance to Certain Foods Yes |
Kidney Stones — |
Marginal Ulcers Yes |
Nausea, Vomiting and/or Stomach Cramps Yes |
Organ Injury During Surgery Yes |
Peritonitis Yes |
Pneumonia Yes |
Port Problems (port flip/ inversion or dislodgement, port leak, port infection, port dislocation) — |
Pouch Dilation — |
Pulmonary Embolism Yes |
Respiratory Failure Yes |
Skin Changes (e.g. acne, dry skin, sagging skin, etc.) Yes |
Stenosis/Stricture About 1% of patients |
Stoma Obstruction — |
Stroke Yes |
Thrombophlebitis Yes |
Thrush (Yeast Infection) Yes |
Vitamin & Mineral Deficiency / Malnutrition / Malabsorption Yes |
Weight Regain Yes |
Wound Reopening Yes |
Wound Sepsis Yes |
Issue Bypass |
Abdominal Discomfort — |
Abdominal hernia Yes |
Abscess Yes |
Anemia Yes |
Band Problems (band erosion, band infection, band intolerance, band leak, band slippage) — |
Blood Clots Yes |
Body Aches Yes |
Body Feeling Changes Yes |
Bowel Function Changes (diarrhea, constipation, foul-smelling bowel movements and flatulence, difficulty swallowing, gurgling noises) Yes |
Bowel Obstruction About 3% of patients |
Deep Vein Thrombosis Yes |
Dehydration Yes |
Dental Problems Yes |
Dumping Syndrome About 70% of patients |
Dyspepsia (Indigestion) Yes |
Esophageal Dilation Yes |
Esophagitis Yes |
Evisceration & Incisional Hernia Yes |
Food Trapping Up to 2% of patients |
Gallstones Up to 1/3 of bariatric patients |
Gastric Fistula Yes |
Gastritis Yes |
Gastroesophageal Reflux Disease (GERD) Yes |
Gastrointestinal Leaks About 2% of patients |
General Anesthesia Complications Yes |
Hair Loss Yes |
Heart Attack Yes |
Hemorrhage (Bleeding) About 2% of patients |
Hiatal Hernia Yes |
Hypoglycemia Yes |
Infection About 3% of patients |
Intolerance to Certain Foods Yes |
Kidney Stones Yes |
Marginal Ulcers Yes |
Nausea, Vomiting and/or Stomach Cramps Up to 70% of patients |
Organ Injury During Surgery Yes |
Peritonitis Yes |
Pneumonia Yes |
Port Problems (port flip/ inversion or dislodgement, port leak, port infection, port dislocation) — |
Pouch Dilation — |
Pulmonary Embolism Yes |
Respiratory Failure Yes |
Skin Changes (e.g. acne, dry skin, sagging skin, etc.) Yes |
Stenosis/Stricture About 5% of patients |
Stoma Obstruction — |
Stroke Yes |
Thrombophlebitis Yes |
Thrush (Yeast Infection) Yes |
Vitamin & Mineral Deficiency / Malnutrition / Malabsorption Yes |
Weight Regain Yes |
Wound Reopening Yes |
Wound Sepsis Yes |
Issue Balloon |
Abdominal Discomfort — |
Abdominal hernia — |
Abscess — |
Anemia — |
Band Problems (band erosion, band infection, band intolerance, band leak, band slippage) — |
Blood Clots — |
Body Aches — |
Body Feeling Changes Yes |
Bowel Function Changes (diarrhea, constipation, foul-smelling bowel movements and flatulence, difficulty swallowing, gurgling noises) — |
Bowel Obstruction — |
Deep Vein Thrombosis — |
Dehydration — |
Dental Problems — |
Dumping Syndrome — |
Dyspepsia (Indigestion) — |
Esophageal Dilation — |
Esophagitis — |
Evisceration & Incisional Hernia — |
Food Trapping — |
Gallstones — |
Gastric Fistula — |
Gastritis — |
Gastroesophageal Reflux Disease (GERD) — |
Gastrointestinal Leaks — |
General Anesthesia Complications — |
Hair Loss — |
Heart Attack — |
Hemorrhage (Bleeding) — |
Hiatal Hernia — |
Hypoglycemia — |
Infection — |
Intolerance to Certain Foods Yes |
Kidney Stones — |
Marginal Ulcers Yes |
Nausea, Vomiting and/or Stomach Cramps Yes |
Organ Injury During Surgery Yes |
Peritonitis Yes |
Pneumonia — |
Port Problems (port flip/ inversion or dislodgement, port leak, port infection, port dislocation) — |
Pouch Dilation — |
Pulmonary Embolism — |
Respiratory Failure — |
Skin Changes (e.g. acne, dry skin, sagging skin, etc.) — |
Stenosis/Stricture — |
Stoma Obstruction Yes |
Stroke — |
Thrombophlebitis — |
Thrush (Yeast Infection) — |
Vitamin & Mineral Deficiency / Malnutrition / Malabsorption — |
Weight Regain Yes |
Wound Reopening — |
Wound Sepsis — |
Issue Band |
Abdominal Discomfort — |
Abdominal hernia Yes |
Abscess Yes |
Anemia — |
Band Problems (band erosion, band infection, band intolerance, band leak, band slippage) Up to 18% of patients |
Blood Clots Yes |
Body Aches Yes |
Body Feeling Changes Yes |
Bowel Function Changes (diarrhea, constipation, foul-smelling bowel movements and flatulence, difficulty swallowing, gurgling noises) Yes |
Bowel Obstruction Yes |
Deep Vein Thrombosis Yes |
Dehydration Yes |
Dental Problems — |
Dumping Syndrome — |
Dyspepsia (Indigestion) Yes |
Esophageal Dilation About 14% of patients |
Esophagitis Yes |
Evisceration & Incisional Hernia Yes |
Food Trapping — |
Gallstones Up to 1/3 of bariatric patients |
Gastric Fistula Yes |
Gastritis Yes |
Gastroesophageal Reflux Disease (GERD) Yes |
Gastrointestinal Leaks — |
General Anesthesia Complications Yes |
Hair Loss Yes |
Heart Attack Yes |
Hemorrhage (Bleeding) Yes |
Hiatal Hernia Yes |
Hypoglycemia — |
Infection Yes |
Intolerance to Certain Foods Yes |
Kidney Stones — |
Marginal Ulcers — |
Nausea, Vomiting and/or Stomach Cramps Yes |
Organ Injury During Surgery Yes |
Peritonitis — |
Pneumonia Yes |
Port Problems (port flip/ inversion or dislodgement, port leak, port infection, port dislocation) About 21% of patients |
Pouch Dilation Up to 17% of patients |
Pulmonary Embolism Yes |
Respiratory Failure Yes |
Skin Changes (e.g. acne, dry skin, sagging skin, etc.) Yes |
Stenosis/Stricture — |
Stoma Obstruction Yes |
Stroke Yes |
Thrombophlebitis Yes |
Thrush (Yeast Infection) Yes |
Vitamin & Mineral Deficiency / Malnutrition / Malabsorption Yes |
Weight Regain Yes |
Wound Reopening Yes |
Wound Sepsis Yes |
Issue DS |
Abdominal Discomfort — |
Abdominal hernia Yes |
Abscess Yes |
Anemia Yes |
Band Problems (band erosion, band infection, band intolerance, band leak, band slippage) Yes |
Blood Clots Yes |
Body Aches Yes |
Body Feeling Changes Yes |
Bowel Function Changes (diarrhea, constipation, foul-smelling bowel movements and flatulence, difficulty swallowing, gurgling noises) Yes |
Bowel Obstruction Yes |
Deep Vein Thrombosis Yes |
Dehydration Yes |
Dental Problems Yes |
Dumping Syndrome — |
Dyspepsia (Indigestion) Yes |
Esophageal Dilation Yes |
Esophagitis Yes |
Evisceration & Incisional Hernia Yes |
Food Trapping — |
Gallstones Up to 1/3 of bariatric patients |
Gastric Fistula Yes |
Gastritis Yes |
Gastroesophageal Reflux Disease (GERD) Yes |
Gastrointestinal Leaks Yes |
General Anesthesia Complications Yes |
Hair Loss Yes |
Heart Attack Yes |
Hemorrhage (Bleeding) Yes |
Hiatal Hernia Yes |
Hypoglycemia — |
Infection Yes |
Intolerance to Certain Foods Yes |
Kidney Stones Yes |
Marginal Ulcers Yes |
Nausea, Vomiting and/or Stomach Cramps Yes |
Organ Injury During Surgery Yes |
Peritonitis Yes |
Pneumonia Yes |
Port Problems (port flip/ inversion or dislodgement, port leak, port infection, port dislocation) — |
Pouch Dilation — |
Pulmonary Embolism Yes |
Respiratory Failure Yes |
Skin Changes (e.g. acne, dry skin, sagging skin, etc.) Yes |
Stenosis/Stricture Yes |
Stoma Obstruction — |
Stroke Yes |
Thrombophlebitis Yes |
Thrush (Yeast Infection) Yes |
Vitamin & Mineral Deficiency / Malnutrition / Malabsorption Yes |
Weight Regain Yes |
Wound Reopening Yes |
Wound Sepsis Yes |
Issue vBloc |
Abdominal Discomfort — |
Abdominal hernia — |
Abscess Yes |
Anemia — |
Band Problems (band erosion, band infection, band intolerance, band leak, band slippage) — |
Blood Clots Yes |
Body Aches Yes |
Body Feeling Changes Yes |
Bowel Function Changes (diarrhea, constipation, foul-smelling bowel movements and flatulence, difficulty swallowing, gurgling noises) — |
Bowel Obstruction — |
Deep Vein Thrombosis — |
Dehydration — |
Dental Problems — |
Dumping Syndrome — |
Dyspepsia (Indigestion) — |
Esophageal Dilation — |
Esophagitis — |
Evisceration & Incisional Hernia Yes |
Food Trapping — |
Gallstones — |
Gastric Fistula Yes |
Gastritis — |
Gastroesophageal Reflux Disease (GERD) — |
Gastrointestinal Leaks — |
General Anesthesia Complications Yes |
Hair Loss — |
Heart Attack Yes |
Hemorrhage (Bleeding) Yes |
Hiatal Hernia — |
Hypoglycemia — |
Infection Yes |
Intolerance to Certain Foods — |
Kidney Stones — |
Marginal Ulcers — |
Nausea, Vomiting and/or Stomach Cramps — |
Organ Injury During Surgery Yes |
Peritonitis — |
Pneumonia Yes |
Port Problems (port flip/ inversion or dislodgement, port leak, port infection, port dislocation) — |
Pouch Dilation — |
Pulmonary Embolism Yes |
Respiratory Failure Yes |
Skin Changes (e.g. acne, dry skin, sagging skin, etc.) — |
Stenosis/Stricture — |
Stoma Obstruction — |
Stroke Yes |
Thrombophlebitis Yes |
Thrush (Yeast Infection) Yes |
Vitamin & Mineral Deficiency / Malnutrition / Malabsorption — |
Weight Regain Yes |
Wound Reopening Yes |
Wound Sepsis Yes |
Issue AspireAssist |
Abdominal Discomfort Yes |
Abdominal hernia — |
Abscess — |
Anemia — |
Band Problems (band erosion, band infection, band intolerance, band leak, band slippage) — |
Blood Clots — |
Body Aches — |
Body Feeling Changes — |
Bowel Function Changes (diarrhea, constipation, foul-smelling bowel movements and flatulence, difficulty swallowing, gurgling noises) Yes |
Bowel Obstruction — |
Deep Vein Thrombosis — |
Dehydration — |
Dental Problems — |
Dumping Syndrome — |
Dyspepsia (Indigestion) — |
Esophageal Dilation — |
Esophagitis — |
Evisceration & Incisional Hernia — |
Food Trapping — |
Gallstones — |
Gastric Fistula — |
Gastritis — |
Gastroesophageal Reflux Disease (GERD) — |
Gastrointestinal Leaks — |
General Anesthesia Complications — |
Hair Loss — |
Heart Attack — |
Hemorrhage (Bleeding) — |
Hiatal Hernia — |
Hypoglycemia — |
Infection Yes |
Intolerance to Certain Foods — |
Kidney Stones — |
Marginal Ulcers Yes |
Nausea, Vomiting and/or Stomach Cramps Yes |
Organ Injury During Surgery — |
Peritonitis — |
Pneumonia — |
Port Problems (port flip/ inversion or dislodgement, port leak, port infection, port dislocation) — |
Pouch Dilation — |
Pulmonary Embolism — |
Respiratory Failure — |
Skin Changes (e.g. acne, dry skin, sagging skin, etc.) — |
Stenosis/Stricture — |
Stoma Obstruction Yes |
Stroke — |
Thrombophlebitis — |
Thrush (Yeast Infection) — |
Vitamin & Mineral Deficiency / Malnutrition / Malabsorption — |
Weight Regain — |
Wound Reopening — |
Wound Sepsis — |
For definitions of any issue in the chart, see our Bariatric Surgery Complications page.
Preventing Complications
In many cases, complications after any type of bariatric surgery arise because the patient didn’t follow their doctor’s instructions.
Behaviors that will dramatically reduce your risk of complications include:
- Pick a good surgeon
- Follow your surgical team’s advice to the letter
- Educate yourself
- Educate your family
- Lose as much weight as possible prior to surgery
- Eat a healthy diet in the months leading up to surgery
- Get tested for sleep apnea syndrome several weeks before surgery (and address the issue if it exists before moving forward)
- Plan for at least 2 weeks of recovery time
- Exercise as quickly as possible after surgery, starting slowly at first and working your way up
- Use compression stockings, pneumatic compression devices, and/or blood thinners after surgery (talk with your surgeon) to reduce risk of blood clots (for all procedures except gastric balloon)
- Have an effective support system of friends, family, and weight loss surgery support groups
Side Effects: Digestion & Sagging Skin
Side Effects: Digestion & Sagging Skin
Digestion Issues
Digestion issues are possible after all procedures except vBloc Therapy. Most of the following issues are avoidable with the right diet and lifestyle changes:
Bowel Movement Problems Bowel Movement Problems |
Difficulty Swallowing Difficulty Swallowing |
Indigestion (Dyspepsia) Indigestion (Dyspepsia) |
Gallstones Gallstones |
Gastroesophageal Reflux Disease (GERD) Gastroesophageal Reflux Disease (GERD) |
Intolerance to certain foods Intolerance to certain foods |
Nausea and vomiting Nausea and vomiting |
Vitamin and/or mineral deficiency Vitamin and/or mineral deficiency |
Sleeve |
Bowel Movement Problems Yes |
Difficulty Swallowing Yes |
Indigestion (Dyspepsia) Yes |
Gallstones Yes |
Gastroesophageal Reflux Disease (GERD) Yes |
Intolerance to certain foods Yes |
Nausea and vomiting Yes |
Vitamin and/or mineral deficiency Unlikely |
Bypass |
Bowel Movement Problems Yes |
Difficulty Swallowing Yes |
Indigestion (Dyspepsia) Yes |
Gallstones Yes |
Gastroesophageal Reflux Disease (GERD) Yes |
Intolerance to certain foods Yes |
Nausea and vomiting Yes |
Vitamin and/or mineral deficiency Yes |
DS |
Bowel Movement Problems Yes |
Difficulty Swallowing Yes |
Indigestion (Dyspepsia) Yes |
Gallstones Yes |
Gastroesophageal Reflux Disease (GERD) Yes |
Intolerance to certain foods Yes |
Nausea and vomiting Yes |
Vitamin and/or mineral deficiency Yes |
Band |
Bowel Movement Problems Yes |
Difficulty Swallowing No |
Indigestion (Dyspepsia) Yes |
Gallstones Yes |
Gastroesophageal Reflux Disease (GERD) Yes |
Intolerance to certain foods Yes |
Nausea and vomiting Yes |
Vitamin and/or mineral deficiency Unlikely |
Balloon |
Bowel Movement Problems Yes |
Difficulty Swallowing Yes |
Indigestion (Dyspepsia) No |
Gallstones No |
Gastroesophageal Reflux Disease (GERD) No |
Intolerance to certain foods Yes |
Nausea and vomiting Yes |
Vitamin and/or mineral deficiency No |
vBloc |
Bowel Movement Problems No |
Difficulty Swallowing No |
Indigestion (Dyspepsia) No |
Gallstones No |
Gastroesophageal Reflux Disease (GERD) No |
Intolerance to certain foods No |
Nausea and vomiting No |
Vitamin and/or mineral deficiency No |
AspireAssist |
Bowel Movement Problems Yes |
Difficulty Swallowing No |
Indigestion (Dyspepsia) No |
Gallstones No |
Gastroesophageal Reflux Disease (GERD) No |
Intolerance to certain foods No |
Nausea and vomiting Yes |
Vitamin and/or mineral deficiency Possibly |
Sagging Skin
Sagging skin is an issue for most patients who lose a lot of weight quickly, especially after the more involved procedures like gastric sleeve, gastric bypass, duodenal switch, and Lap-Band.
It is less likely after gastric balloon and vBloc therapy because patients tend to not lose as much weight after those procedures.
Weight Regain
Five to ten percent weight regain is common after most procedures, although it is much less likely after duodenal switch surgery due to that procedure’s unique combination of restriction and malabsorption.
Weight regain is usually the result of patients not following proper diet guidelines.
Revision Surgery
Available for Most Procedures
Revision Surgery: Available for Most Procedures
Revision surgery may be an option for gastric sleeve, gastric bypass, duodenal switch, Lap-Band, vBloc Therapy, or AspireAssist patients who:
- Regain weight after surgery
- Have a complication that requires it
Revisions are not available for gastric balloon patients because the balloon is removed after 6 months regardless of weight loss. However, many balloon patients convert to a more involved procedure to help continue weight loss after the balloon is removed.
Summary
Full Comparison & Procedure Patient Guides
Your individual situation will determine which type of bariatric surgery is best for you. Unfortunately, there is no “one size fits all” option. Following is a review of winners in each category:
Most Weight Loss
- Winner: Duodenal Switch
- Runners Up: (Tie) Gastric Sleeve & Gastric Bypass
Best Health Improvement
- Winner: Duodenal Switch
- Runners Up: (Tie) Gastric Sleeve & Gastric Bypass
Easiest to Qualify
- Winner: No Clear Winner; Depends on Your Current BMI
Low-Cost Procedure (Without Insurance)
- Winner: Gastric Balloon (but long-term costs likely higher than more expensive procedures)
- Runners Up: Lap Band (but long-term costs likely higher than more expensive procedures)
Low-Cost Procedure (With Insurance)
- Winner: 4-Way Tie – Gastric Sleeve, Gastric Bypass, Duodenal Switch, & Lap-Band
- Runners Up: Gastric Balloon
Insurance Coverage
- Winner: (4-Way Tie) Sleeve, Bypass, Band, & Duodenal Switch
Most Popular Procedure
- Winner: Gastric Sleeve
- Runners Up: Gastric Bypass
Quickest Recovery
- Winner: (Tie) vBloc Therapy, Gastric Balloon & AspireAssist
- Runners Up: Lap-Band
Best Post-Op Diet
- Winner: Depends on Patient’s Goals; Easier Diet’s Usually Mean Less Weight Loss
Fewest Risks & Side Effects
- Winner: vBloc Therapy
- Runners Up: (Tie) Gastric Balloon & Gastric Sleeve
Overall Winner for You
- Winner:Take the Choose My Procedure Quiz
- Runners Up:Take the Choose My Procedure Quiz
Help & Support
Patient Experiences & Ask the Expert
Patient Experiences & Ask the Expert
If you still have questions about the type of bariatric surgery, our experts are happy to answer them. We (and other patients) would also love to hear about your experiences with the balloon.
Please use the form below to share your experience or ask a question.
Questions From Other Visitors*
Click below to see contributions from other visitors to this page.


