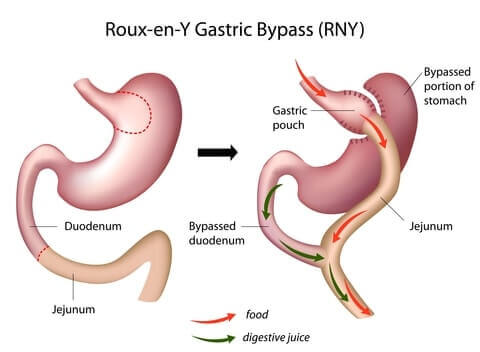
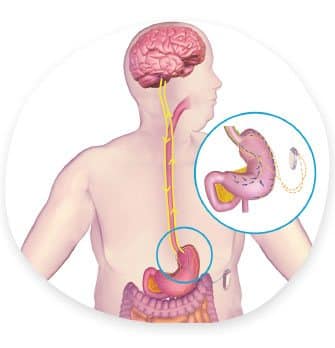
Gastric bypass surgery (“Roux-en-Y gastric bypass”) makes the stomach smaller and reroutes the intestines. As a result, patients:
- Feel full sooner after eating
- Absorb less food
- Lose up to two-thirds of their excess weight within 2 years
- Have significant health improvement
This page covers everything you need to determine whether gastric bypass is the right weight loss procedure for you.

Weight Loss
Half to Most of Your Excess Weight 
Weight Loss – Half to Most of Your Excess Weight
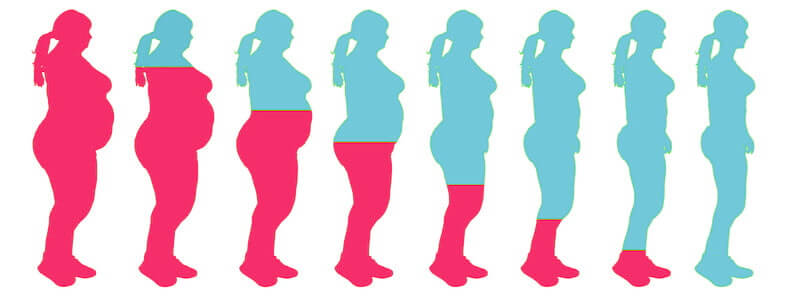
Gastric bypass patients usually lose a lot of weight very quickly. Within 3 months, the average patient will lose about one-third of their excess weight. By the one-year mark, almost two-thirds of the excess weight will be gone.
Many patients reach “peak” weight loss between one and two years, then gain a little back (more about Weight Regain in the “Downsides” section below). But long-term results are still impressive, with the average patient keeping about 60% of their excess weight off.
Gastric Bypass Weight Loss Studies
Summary of Findings When Comparing Gastric Bypass to Other Procedures Summary of Findings When Comparing Gastric Bypass to Other Procedures |
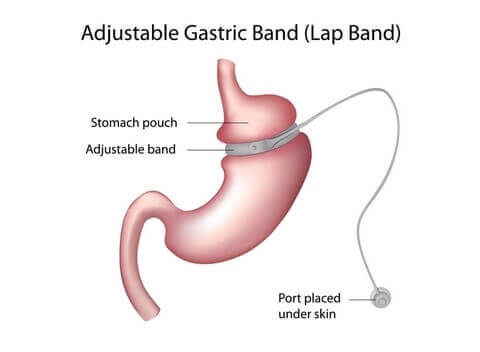
Lap Band Surgery vs Gastric Bypass Lap Band Surgery vs Gastric Bypass |
Roux-en-Y gastric bypass is associated with better weight loss, resulting in a better correction of some comorbidities than gastric banding, at the price of a higher early complication rate. This difference, however, is largely compensated by the much higher long-term complication and reoperation rates seen after gastric banding.O Roux-en-Y gastric bypass is associated with better weight loss, resulting in a better correction of some comorbidities than gastric banding, at the price of a higher early complication rate. This difference, however, is largely compensated by the much higher long-term complication and reoperation rates seen after gastric banding.O |
Weight loss outcomes strongly favored gastric bypass over lap band surgery. Patients treated with lap band had lower short-term morbidity than those treated with gastric bypass, but reoperation rates were higher among patients who received lap band surgery. Gastric bypass should remain the primary bariatric procedure used to treat obesity in the United States.A Editor’s Note: This study was published before long-term results had been published for gastric sleeve surgery. Weight loss outcomes strongly favored gastric bypass over lap band surgery. Patients treated withlap band had lower short-term morbidity than those treated with gastric bypass, but reoperation rates were higher among patients who receivedlap band surgery. Gastric bypass should remain the primary bariatric procedure used to treat obesity in the United States.A Editor’s Note: This study was published before long-term results had been published for gastric sleeve surgery. |
Collectively, data clearly point to distinct changes in dietary habits after bariatric operations which markedly differ between gastric bypass andlap band patients. Overall, it is tempting to conclude that gastric bypass operations lead to a healthier and a more balanced diet thanlap band implantations.B Collectively, data clearly point to distinct changes in dietary habits after bariatric operations which markedly differ between gastric bypass andlap band patients. Overall, it is tempting to conclude that gastric bypass operations lead to a healthier and a more balanced diet thanlap band implantations.B |
Gastric bypass seems to provide a stronger suppression of ghrelin in comparison with gastric lap band procedure. These findings are consistent with the hypothesis that suppression of ghrelin is one mechanism by which gastric bypass can reduce body weight long term, more thanlap band.C Gastric bypass seems to provide a stronger suppression of ghrelin in comparison with gastric lap band procedure. These findings are consistent with the hypothesis that suppression of ghrelin is one mechanism by which gastric bypass can reduce body weight long term, more thanlap band.C |
Mini Gastric Bypass Surgery vs Gastric Bypass Mini Gastric Bypass Surgery vs Gastric Bypass |
Pending long-term evaluation, mini gastric bypass surgery seems a good alternative to gastric bypass, giving the same results with a more simple and reproducible technique.D Pending long-term evaluation, mini gastric bypass surgery seems a good alternative to gastric bypass, giving the same results with a more simple and reproducible technique.D |
Previous studies have demonstrated that hospitalization after gastric bypass increases remarkably (20% per year). The present study shows that hospitalization followingmini gastric bypass surgery instead of rising, as reported with gastric bypass, decreases by a third. Themini gastric bypass has been shown to be a short, safe successful weight loss surgery in previous work. The present study supports themini gastric bypass as a low risk procedure that decreases the need for hospitalization.E Previous studies have demonstrated that hospitalization after gastric bypass increases remarkably (20% per year). The present study shows that hospitalization followingmini gastric bypass surgery instead of rising, as reported with gastric bypass, decreases by a third. Themini gastric bypass has been shown to be a short, safe successful weight loss surgery in previous work. The present study supports themini gastric bypass as a low risk procedure that decreases the need for hospitalization.E |
Both gastric bypass andmini gastric bypass surgery are effective for morbid obesity with similar results for resolution of metabolic syndrome and improvement of quality of life. Mini gastric bypass surgery is a simpler and safer procedure that has no disadvantage compared with gastric bypass at 2 years of follow-up.F Both gastric bypass andmini gastric bypass surgery are effective for morbid obesity with similar results for resolution of metabolic syndrome and improvement of quality of life. Mini gastric bypass surgery is a simpler and safer procedure that has no disadvantage compared with gastric bypass at 2 years of follow-up.F |
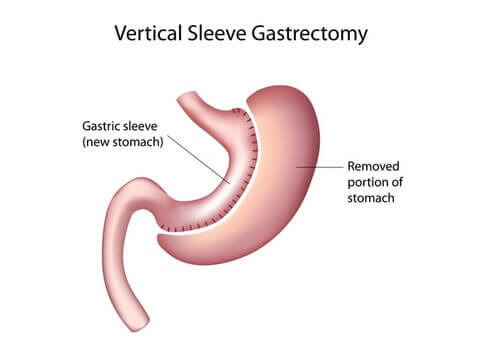
Gastric Sleeve Surgery vs Gastric Bypass Gastric Sleeve Surgery vs Gastric Bypass |
Compared with gastric sleeve, gastric bypass had significantly better effect in resolving type 2 diabetes mellitus, hypertension, hypercholesterolemia, gastroesophageal reflux disease, and arthritis. However, gastric bypass had higher incidence of complications and reoperation, and longer operation time than gastric sleeve.P Compared with gastric sleeve, gastric bypass had significantly better effect in resolving type 2 diabetes mellitus, hypertension, hypercholesterolemia, gastroesophageal reflux disease, and arthritis. However, gastric bypass had higher incidence of complications and reoperation, and longer operation time than gastric sleeve.P |
Overall complication rates among patients undergoing gastric sleeve (SG) (6.3%) were significantly lower than for gastric bypass (RYGB) (10.0%, P < 0.0001). Serious complication rates were similar for SG (2.4%) and RYGB (2.5%, P = 0.736). Excess body weight loss at 1 year was 13% lower for SG (60%) than for RYGB (69%, P < 0.0001). SG was closer to RYGB than lap band (LAGB) with regard to remission of obesity-related comorbidities.Q Overall complication rates among patients undergoing gastric sleeve (SG) (6.3%) were significantly lower than for gastric bypass (RYGB) (10.0%, P < 0.0001). Serious complication rates were similar for SG (2.4%) and RYGB (2.5%, P = 0.736). Excess body weight loss at 1 year was 13% lower for SG (60%) than for RYGB (69%, P < 0.0001). SG was closer to RYGB than lap band (LAGB) with regard to remission of obesity-related comorbidities.Q |
PYY levels increased similarly after either procedure. The markedly reduced ghrelin levels in addition to increased PYY levels after gastric sleeve surgery, are associated with greater appetite suppression and excess weight loss compared with gastric bypass.I (Editors’s note: both ghrelin and peptide YY effect appetite. See our obesity and genetics page for more details) PYY levels increased similarly after either procedure. The markedly reduced ghrelin levels in addition to increased PYY levels after gastric sleeve surgery, are associated with greater appetite suppression and excess weight loss compared with gastric bypass.I (Editors’s note: both ghrelin and peptide YY effect appetite. See our obesity and genetics page for more details) |
The gastric sleeve operation is able to achieve significant weight loss comparable to the gastric bypass and duodenal switch operations but with the low morbidity profile similar to that of lap band placement.J The gastric sleeve operation is able to achieve significant weight loss comparable to the gastric bypass and duodenal switch operations but with the low morbidity profile similar to that of lap band placement.J |
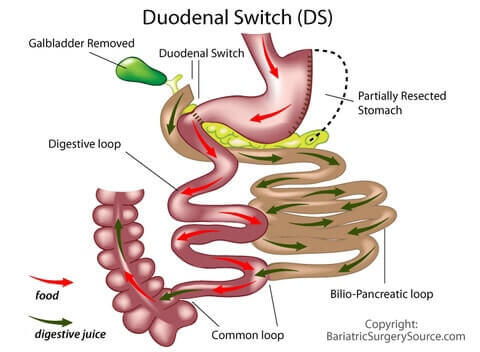
Duodenal Switch (DS) vs Gastric Bypass Duodenal Switch (DS) vs Gastric Bypass |
Compared with gastric bypass, duodenal switch may be associated with a greater risk of vitamin A and D deficiencies in the first year after surgery and of thiamine deficiency in the initial months after surgery.K(Editors’s note: See our Bariatric Vitamins page for more.) Compared with gastric bypass, duodenal switch may be associated with a greater risk of vitamin A and D deficiencies in the first year after surgery and of thiamine deficiency in the initial months after surgery.K(Editors’s note: See our Bariatric Vitamins page for more.) |
Although duodenal switch is associated with more bowel episodes than gastric bypass, the difference is not statistically significant. Bowel habits are similar in patients who achieve 50% estimated body weight loss with duodenal switch surgery or gastric bypass.L Although duodenal switch is associated with more bowel episodes than gastric bypass, the difference is not statistically significant. Bowel habits are similar in patients who achieve 50% estimated body weight loss with duodenal switch surgery or gastric bypass.L |
Direct comparison of Duodenal Switch toGastric Bypass demonstrates superior weight loss outcomes for DS. Importantly, the likelihood of successful weight loss (excess weight loss >50%) was significantly greater in patients following DS (12 months, 83.9% vs. 70.4%; 18 months, 90.3% vs. 75.9%; 36 months, 84.2% vs. 59.3%).M Direct comparison of Duodenal Switch toGastric Bypass demonstrates superior weight loss outcomes for DS. Importantly, the likelihood of successful weight loss (excess weight loss >50%) was significantly greater in patients following DS (12 months, 83.9% vs. 70.4%; 18 months, 90.3% vs. 75.9%; 36 months, 84.2% vs. 59.3%).M |
No patients reported dumping syndrome (after DS surgery), and marginal ulcers were not seen.N No patients reported dumping syndrome (after DS surgery), and marginal ulcers were not seen.N |
Summary of Findings When Comparing Gastric Bypass to Other Procedures Year of Study |
Lap Band Surgery vs Gastric Bypass |
Roux-en-Y gastric bypass is associated with better weight loss, resulting in a better correction of some comorbidities than gastric banding, at the price of a higher early complication rate. This difference, however, is largely compensated by the much higher long-term complication and reoperation rates seen after gastric banding.O 2012 |
Weight loss outcomes strongly favoredgastric bypass over lap band surgery. Patients treated withlap band had lower short-term morbidity than those treated with gastric bypass, but reoperation rates were higher among patients who receivedlap band surgery. Gastric bypass should remain the primary bariatric procedure used to treat obesity in the United States.A Editor’s Note: This study was published before long-term results had been published for gastric sleeve surgery. 2008 |
Collectively, data clearly point to distinct changes in dietary habits after bariatric operations which markedly differ between gastric bypass andlap band patients. Overall, it is tempting to conclude that gastric bypass operations lead to a healthier and a more balanced diet thanlap band implantations.B 2008 |
Gastric bypass seems to provide a stronger suppression of ghrelin in comparison with gastric lap band procedure. These findings are consistent with the hypothesis that suppression of ghrelin is one mechanism by which gastric bypass can reduce body weight long term, more thanlap band.C 2003 |
Mini Gastric Bypass Surgery vs Gastric Bypass |
Pending long-term evaluation, mini gastric bypass surgery seems a good alternative to gastric bypass, giving the same results with a more simple and reproducible technique.D 2008 |
Previous studies have demonstrated that hospitalization after gastric bypass increases remarkably (20% per year). The present study shows that hospitalization followingmini gastric bypass surgery instead of rising, as reported with gastric bypass, decreases by a third. Themini gastric bypass has been shown to be a short, safe successful weight loss surgery in previous work. The present study supports themini gastric bypass as a low risk procedure that decreases the need for hospitalization.E 2006 |
Both gastric bypass andmini gastric bypass surgery are effective for morbid obesity with similar results for resolution of metabolic syndrome and improvement of quality of life. Mini gastric bypass surgery is a simpler and safer procedure that has no disadvantage compared with gastric bypass at 2 years of follow-up.F 2005 |
Gastric Sleeve Surgery vs Gastric Bypass |
Compared with gastric sleeve, gastric bypass had significantly better effect in resolving type 2 diabetes mellitus, hypertension, hypercholesterolemia, gastroesophageal reflux disease, and arthritis. However, gastric bypass had higher incidence of complications and reoperation, and longer operation time than gastric sleeve.P 2014 |
Overall complication rates among patients undergoing gastric sleeve (SG) (6.3%) were significantly lower than for gastric bypass (RYGB) (10.0%, P < 0.0001). Serious complication rates were similar for SG (2.4%) and RYGB (2.5%, P = 0.736). Excess body weight loss at 1 year was 13% lower for SG (60%) than for RYGB (69%, P < 0.0001). SG was closer to RYGB than lap band (LAGB) with regard to remission of obesity-related comorbidities.Q 2013 |
PYY levels increased similarly after either procedure. The markedly reduced ghrelin levels in addition to increased PYY levels after gastric sleeve surgery, are associated with greater appetite suppression and excess weight loss compared with gastric bypass.I (Editors’s note: both ghrelin and peptide YY effect appetite. See our obesity and genetics page for more details) 2008 |
The gastric sleeve operation is able to achieve significant weight loss comparable to the gastric bypass and duodenal switch operations but with the low morbidity profile similar to that of lap band placement.J 2007 |
Duodenal Switch (DS) vs Gastric Bypass |
Compared with gastric bypass, duodenal switch may be associated with a greater risk of vitamin A and D deficiencies in the first year after surgery and of thiamine deficiency in the initial months after surgery.K(Editors’s note: See our Bariatric Vitamins page for more.) 2009 |
Although duodenal switch is associated with more bowel episodes than gastric bypass, the difference is not statistically significant. Bowel habits are similar in patients who achieve 50% estimated body weight loss with duodenal switch surgery or gastric bypass.L 2008 |
Direct comparison of Duodenal Switch toGastric Bypass demonstrates superior weight loss outcomes for DS. Importantly, the likelihood of successful weight loss (excess weight loss >50%) was significantly greater in patients following DS (12 months, 83.9% vs. 70.4%; 18 months, 90.3% vs. 75.9%; 36 months, 84.2% vs. 59.3%).M 2006 |
No patients reported dumping syndrome (after DS surgery), and marginal ulcers were not seen.N 2006 |
Keep in mind that these are averages – “middle of the road” results. Patients who eat the right foods, exercise regularly, and follow their surgeon’s advice can lose even more, while patients who veer off-track lose less.
Health Benefits
Improves or Cures At Least 15 Conditions
Health Benefits – Improves or Cures At Least 15 Conditions
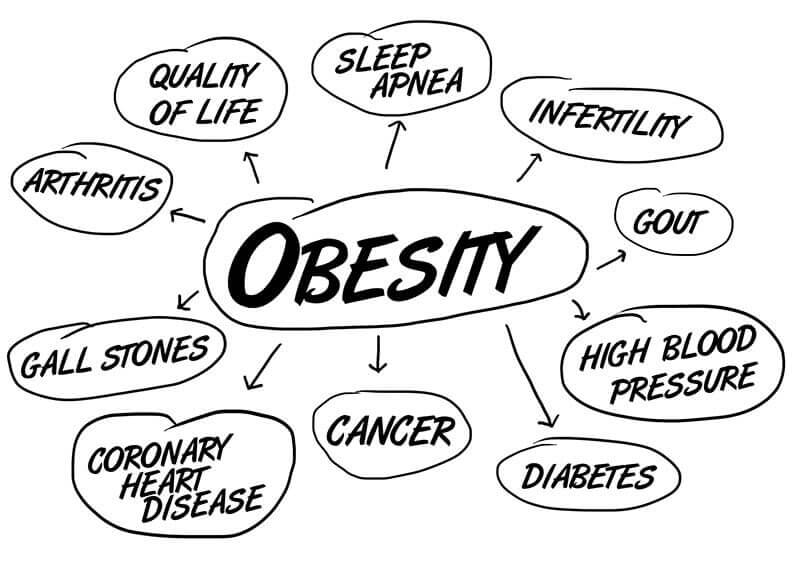
Most gastric bypass patients experience significant improvement in or a complete “cure” of obesity-related health problems, including:
Mortality Reduction/Life Expectancy (5 year mortality)
Dyslipidemia hypercholesterolemia
Gastroesophageal Reflux Disease (GERD)
Hyperlipidemia (high levels of fat in the blood)
Non-Alcoholic Fatty Liver Disease
Qualify
35+ BMI with Health Issues, 40+ Without
Qualify – 35+ BMI with Health Issues, 40+ Without
Most surgeons and insurance companies follow the guidelines of the National Institutes of Health (NIH) which state that you must fall into one of the following categories in order to qualify for gastric bypass surgery:
- Have a body mass index (BMI) of 40 or more (“morbidly obese” or “super obese”), OR
- Have a BMI between 35 and 39.9 (“severely obese”) and have a serious obesity-related health problem
Your Weight Classification:
Below 18.5
Underweight
Your Health Risk:HighYou are considered to be underweight and should take physician-approved steps to gain weight.
18.5 – 24.9
Healthy Weight
Your Health Risk:Low25.0 – 29.9
Overweight
Your Health Risk:MODERATEYour risk increases to “High” if two or more of the following apply to you:
- You smoke cigarettes
- Family history of premature heart disease
- High blood glucose (blood sugar)
- High blood pressure (hypertension)
- Low HDL-cholesterol
(“good” cholesterol) - High LDL-cholesterol
(“bad” cholesterol) - High triglycerides
Your risk of health issues are even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
30.0 – 34.9
Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for weight loss surgery if you also have poorly controlled type 2 diabetes and/or have a higher risk of cardiovascular disease.
Learn Your Options35.0 – 39.9
Severely Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for weight loss surgery if you also have one or more obesity-related health problems.
Learn Your Options40.0 – 49.9
Morbidly Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for weight loss surgery.
Learn Your Options50 or Higher
Super Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for weight loss surgery.
Learn Your Options
Your Weight Classification:
Below 18.5
Underweight
Your Health Risk:HighYou are considered to be underweight and should take physician-approved steps to gain weight.
18.5 – 24.9
Healthy Weight
Your Health Risk:Low25.0 – 29.9
Overweight
Your Health Risk:MODERATEYour risk increases to “High” if two or more of the following apply to you:
- You smoke cigarettes
- Family history of premature heart disease
- High blood glucose (blood sugar)
- High blood pressure (hypertension)
- Low HDL-cholesterol
(“good” cholesterol) - High LDL-cholesterol
(“bad” cholesterol) - High triglycerides
Your risk of health issues are even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
30.0 – 34.9
Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for weight loss surgery if you also have poorly controlled type 2 diabetes and/or have a higher risk of cardiovascular disease.
Learn Your Options35.0 – 39.9
Severely Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for weight loss surgery if you also have one or more obesity-related health problems.
Learn Your Options40.0 – 49.9
Morbidly Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for weight loss surgery.
Learn Your Options50 or Higher
Super Obese
Your Health Risk:HighYou have a very high risk of obesity-related health problems.
Your risk is even higher if your waist circumference is over 35 inches (88 cm) for women or 40 inches (102 cm) for men.
Your BMI indicates that you may be a good candidate for weight loss surgery.
Learn Your Options
Serious obesity-related health problems most commonly include:
- High blood pressure
- High cholesterol
- Type 2 diabetes
- Sleep apnea
Other qualifying health conditions related to obesity are listed in the Health Benefits section above.
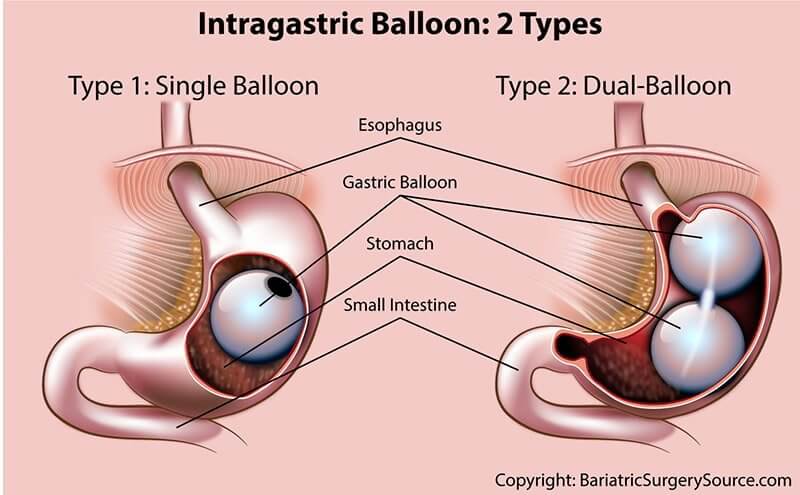
If you do not meet either of these BMI requirements, you still might qualify for one other type of weight loss surgery called Gastric Balloon. See our Gastric Balloon Patient Guide for more information.
Cost
$24,000 Avg Before Discounts, $2,000 Avg With Insurance
Cost – $24,000 Avg Before Discounts, $2,000 Avg With Insurance
On average, the all-in cost of gastric bypass equals (in U.S. Dollars for comparison purposes):
- United States – $24,000 (ranges from $15,000 in Arkansas to $57,000 in Alaska)
- Canada – $20,000
- Australia – $17,000
- Mexico – $7,400
- India – $10,400
- Thailand – $10,500
- Costa Rica – $12,500
However, your out-of-pocket costs depend on several factors including:
- Whether your procedure is open or laparoscopic – open gastric bypass surgery tends to cost about $2,500 more than laparoscopic surgery, on average (33)
- Which hospital you have the surgery in
- Whether or not you have insurance – if your surgeon and hospital are covered by your insurance, it is likely that a discount has been negotiated to allow that surgeon and hospital to participate in your insurance company’s network
- Whether you obtain financing for some or all of the costs
- Specific fees your bariatric surgeon and other professionals charge for the various pre-op, surgical, and post-op services.
Note that the above averages include total costs incurred during surgery. Some surgeons also include Pre-Op costs in their quoted fees (more on Pre-Op and Post-Op fees below).
However, the above averages do not include Post-Op costs which will be based on your specific circumstances.
Click here to see Costs by each US State
|
| ||||
|
| ||||
ALABAMA surgeons surveyed are located in Birmingham, Decatur, Huntsville, Mobile, Montgomery and Tuscaloosa | |||||
|
| ||||
ALASKA surgeons surveyed are located in Anchorage | |||||
|
| ||||
ARIZONA surgeons surveyed are located in Flagstaff, Mesa, Phoenix, Prescott, Scottsdale, Tempe and Tucson | |||||
|
| ||||
ARKANSAS surgeons surveyed are located in El Dorado, Fayetteville, Fort Smith, Jonesboro, Little Rock and Pine Bluff | |||||
|
| ||||
CALIFORNIA surgeons surveyed are located in Bakersfield, Burbank, Chico, Fresno, Los Angeles, Orange, La Jolla, Modesto, Oakland, Poway, Riverside, Sacramento, San Diego, San Francisco, San Jose and Santa Barbara | |||||
|
| ||||
COLORADO surgeons surveyed are located in Colorado Springs, Denver and Fort Collins | |||||
|
| ||||
CONNECTICUT surgeons surveyed are located in Farmington, Glastonbury, Meriden, Middletown, New Haven, Norwalk, Shelton and Stamford | |||||
|
| ||||
DELAWARE surgeons surveyed are located in Dover, Newark and Wilmington | |||||
|
| ||||
FLORIDA surgeons surveyed are located in Ft. Meyers, Gainesville, Jacksonville, Miami, Naples, Ocala, Orlando, Sarasota, St. Petersburg, Tallahassee, Tampa and West Palm Beach | |||||
|
| ||||
GEORGIA surgeons surveyed are located in Albany, Athens, Atlanta, Augusta, Columbus, Decatur, Macon, Marietta and Savannah | |||||
|
| ||||
HAWAII surgeons surveyed are located in Aiea, Kailua-Kona, Honolulu and Wailuku | |||||
|
| ||||
IDAHO surgeons surveyed are located in Boise, Meridian, Montpelier, Nampa, Pocatello and Post Falls | |||||
|
| ||||
ILLINOIS surgeons surveyed are located in Chicago, Champaign, Decatur, Naperville, Peoria, Rockford and Springfield | |||||
|
| ||||
INDIANA surgeons surveyed are located in Bloomington, Evansville, Fort Wayne, Gary, Indianapolis and South Bend | |||||
|
| ||||
IOWA surgeons surveyed are located in Cedar Rapids, Davenport, Des Moines and Iowa City | |||||
|
| ||||
KANSAS surgeons surveyed are located in Topeka, Lenexa, Wichita, Overland Park, Olathe, and Kansas City | |||||
|
| ||||
KENTUCKY surgeons surveyed are located in Lexington, Louisville and other towns. | |||||
|
| ||||
LOUISIANA surgeons surveyed are located in Alexandria, New Orleans, Shreveport and other towns | |||||
|
| ||||
MAINE surgeons surveyed are located in Augusta, Bangor, Portland and other towns | |||||
|
| ||||
MARYLAND surgeons surveyed are located in Baltimore, Salisbury and other towns | |||||
|
| ||||
MASSACHUSETTS surgeons surveyed are located in Boston, New Bedford, Pittsfield, Springfield, Worcester and other towns. | |||||
|
| ||||
MICHIGAN surgeons surveyed are located in Ann Arbor, Detroit, Grand Rapids, Lansing and other towns. | |||||
|
| ||||
MINNESOTA surgeons surveyed are located in Minneapolis / St. Paul, Rochester and other towns | |||||
|
| ||||
MISSISSIPPI surgeons surveyed are located in Jackson, Hattiesburg, Meridian, Tupelo and other towns. | |||||
|
| ||||
MISSOURI surgeons surveyed are located in Columbia, Kansas City, Springfield, St. Louis and other towns | |||||
|
| ||||
MONTANA surgeons surveyed are located in Billings, Bozeman, Helena and other towns | |||||
|
| ||||
NEBRASKA surgeons surveyed are located in Lincoln, Omaha and other towns | |||||
|
| ||||
NEVADA surgeons surveyed are located in Henderson, Las Vegas and Reno Areas | |||||
|
| ||||
NEW HAMPSHIRE surgeons surveyed are located in Manchester, Nashua and other towns | |||||
|
| ||||
NEW JERSEY surgeons surveyed are located in Newark, Trenton and Other Areas | |||||
|
| ||||
NEW MEXICO surgeons surveyed are located in Albuquerque, Las Cruces, Santa Fe and Other Areas | |||||
|
| ||||
NEW YORK surgeons surveyed are located in Albany, Buffalo, New York City / Manhattan, Rochester, Watertown and Other Areas | |||||
|
| ||||
NORTH CAROLINA surgeons surveyed are located in Asheville, Chapel Hill, Charlotte, Durham, Greensboro, Greenville, Raleigh, Wilmington, Winston-Salem and Other Areas | |||||
|
| ||||
NORTH DAKOTA surgeons surveyed are located in Bismarck and Grand Forks | |||||
|
| ||||
OHIO surgeons surveyed are located in Akron, Cincinnati, Cleveland, Columbus, Dayton and Other Areas | |||||
|
| ||||
OKLAHOMA surgeons surveyed are located in Norman, Oklahoma City, Tulsa and Other Areas | |||||
|
| ||||
OREGON surgeons surveyed are located in Portland, Bend, McMinnville, Salem, Medford, Springfield, Eugene, Beaverton, Corvallis, and Coos Bay | |||||
|
| ||||
PENNSYLVANIA surgeons surveyed are located in Allentown, Altoona, Harrisburg, Lancaster, Philadelphia, Pittsburgh and Other Areas | |||||
|
| ||||
SOUTH CAROLINA surgeons surveyed are located in Anderson, Charleston, Columbia, Greenville, Myrtle Beach, Rock Hill and Other Areas | |||||
|
| ||||
SOUTH DAKOTA surgeons surveyed are located in Dakota Dunes, Rapid City and Sioux Falls | |||||
|
| ||||
TENNESSEE surgeons surveyed are located in Chattanooga, Knoxville, Memphis and Nashville | |||||
|
| ||||
TEXAS surgeons surveyed are located in Abilene, Amarillo, Austin, Corpus Christi, Dallas / Ft. Worth, Houston, Lubbock and San Antonio | |||||
|
| ||||
UTAH surgeons surveyed are located in Provo, Salt Lake City and St. George | |||||
|
| ||||
VERMONT surgeons surveyed are located in Burlington, Montpelier and Springfield | |||||
|
| ||||
VIRGINIA surgeons surveyed are located in Charlottesville, Newport News, Norfolk, Richmond, Roanoke, Virginia Beach and Other Towns | |||||
|
| ||||
WASHINGTON surgeons surveyed are located in Everett, Olympia, Seattle, Spokane, Tacoma, Vancouver and Other Areas | |||||
|
| ||||
|
| ||||
WEST VIRGINIA surgeons surveyed are located in Charleston, Huntington, Morgantown and Vienna | |||||
|
| ||||
WISCONSIN surgeons surveyed are located in Eu Claire, Green Bay, La Crosse, Madison, Milwaukee and Other Areas | |||||
|
| ||||
WYOMING surgeons surveyed are located in Afton, Cheyenne and Riverton | |||||
Click here to see Costs by each Australian State/Territory
|
| ||||
|
| ||||
NEW SOUTH WALES surgeons surveyed are located in Sydney | |||||
|
| ||||
QUEENSLAND surgeons surveyed are located in Brisbane and Gold Coast | |||||
|
| ||||
SOUTH AUSTRALIA surgeons surveyed are located in Adelaide and Barossa Valley | |||||
TASMANIA surgeons surveyed are located in Hobart | |||||
|
| ||||
VICTORIA surgeons surveyed are located in Melbourne | |||||
WESTERN AUSTRALIA surgeons surveyed are located in Perth | |||||
Total surgery costs can be further complicated by:
- Self-Pay Discounts – Most weight loss surgery clinics will offer some sort of self-pay discount or payment plan if you don’t have insurance (or if insurance won’t cover the procedure). All you have to do is ask!
- Other Discounts – Additional discounts may be offered for things like full up-front payment. Ask your surgeon’s office if there are any other discounts that you might be able to take advantage of.
- Same Surgeon, Different Hospitals – Some surgeons have “operating privileges” at more than one hospital. Since hospital costs can vary widely – even in the same town and regardless of quality – ask your surgeon if you have a choice.
Gastric bypass fees are split between Pre-Op, Surgery, and Post-Op services:
Pre-Op (Costs Before Surgery)
- Physician-supervised weight loss program (required prior to surgery approval)
- Dietitian/nutritionist consultations
- Psychologist (mental health clearance)
- Cardiologist (heart health clearance)
- Lab/blood work, echocardiogram (also known as an “ECG” or “EKG”) and/or X-Ray fees
- Surgeon consultation fees
- Sleep study
Costs During Surgery
- Hospital fees
- Surgeon fees
- Surgical assistant fees
- Anesthesia fees
- Operating room fees
Post-Op (Costs After Surgery)
- Addressing any complications
- Follow-up doctor visits
- Bariatric vitamins
- Additional food costs (healthier food tends to cost more)
- Personal trainer and/or gym membership
- New clothes (wait to go crazy with this until you reach your plateau weight)
- Plastic surgery to address sagging skin (more on this in the Downsides section below)
Gastric Bypass Costs Vs. Cost of Not Having Surgery
While gastric bypass surgery is costly, the long-term costs of obesity-related health problems for people who don’t get the surgery are even higher.
Compared to morbidly obese people who don’t have surgery, bariatric patients pay off their entire surgery and start getting ahead financially after only 2 years (34).
Fewer prescription drugs alone have been found to save patients $3,000 or more per year (35).
A study published by the American Journal of Managed Care (AJMC) found that bariatric patients pay as much as $900 less per month as soon as 13 months after surgery than similar people who didn’t have surgery (36). That’s almost $11,000 per year in total medical costs saved for bariatric patients versus morbidly obese people who do not have surgery.
Vs. Other Procedures: 2nd Highest of 7 / With Insurance: Tied for Lowest
Gastric bypass has the 2nd highest average cost out of the 7 available types of weight loss surgery, if you don’t have insurance. It is tied for the lowest cost for patients with insurance.
Free Insurance Check & Cost Quote:Click here to contact a gastric bypass surgeon
See our Types of Bariatric Surgery page for a full comparison.
Financing Options
Gastric bypass financing is available in most locations. With no insurance, patients can obtain financing for the entire cost of surgery. With insurance, patients can get assistance with paying large deductibles or other out-of-pocket expenses.
Options for making surgery more affordable include (follow links for more information):
- Payment Plan Through a Qualified Bariatric Surgeon – This is probably your most realistic and affordable local non-insurance option
- Brokers, Direct Lenders and Credit Cards (Unsecured Medical Loans)
- Friends & Family
- Secured Medical Loans
- Retirement Plan Loans
- Permanent Life Insurance Loans
- Medical travel – having surgery in a location that is less expensive than where you live
Taxes: Several Ways to Save
Most countries provide tax benefits to gastric bypass patients who qualify.
United States: Might Be Deductible
Gastric bypass surgery is tax deductible as long as the costs are higher than 10% of your adjusted gross income (click here for IRS rules).
In order to receive the deductions, you’ll need to complete Schedule A of the IRS Form 1040. You’ll also need to save your medical bills and payment statements as proof. Note that any reimbursed amounts cannot be included (such as the amount that insurance paid).
Depending on your employment status, money accrued in special savings accounts (or even your IRA) could also be a tax-advantaged payment option. Special tax-favored accounts to consider include:
- Health Savings Account (HSA) – HSAs can only be opened alongside a “qualified high deductible” health plan. Money contributed to an HSA, accumulated interest from the accounts where the money is invested, AND money taken out of the HSA to pay for qualified medical expenses are all TAX FREE. No other account receives more favorable tax treatment. You may even be able to transfer money already in your IRA into an HSA. See the IRS’s Site for more info.
- Archer Medical Savings Account (Archer MSA) – Archer MSAs are very similar to HSAs, except they are for self-employed individuals or small businesses. Click here for the details.
- Health Reimbursement Account (HRA) – HRAs can only be offered by your employer, and only your employer can contribute money to them. If your company offers one, make sure your plan allows the use of HRA funds to pay for “all qualified medical expenses” as financing bariatric surgery is not allowed with some plans. More information can be found by clicking here.
- Flexible Spending Account (FSA) – Both employers and employees can contribute to an FSA, also known by its IRS code, “Section 125”. FSA’s can be offered alongside any health plan, and withdrawals from this account can be made tax-free as long as they are used to pay for qualified medical expenses. Click here to get the summary from the IRS.
Canada: Is Deductible
Canada is generous compared to other countries when it comes to medical tax deductions. As long as you can substantiate your out of pocket gastric bypass expenses with a prescription, receipt, or other documentation, you should be able to write them off.
If your surgery is covered by insurance, you can also deduct your monthly insurance premiums.
If your income is below a certain threshold, you may qualify for a tax credit called the refundable medical expense supplement.
Australia: Might Be Deductible
If your out of pocket expenses for bariatric surgery (and all other net medical expenses) are over the Australian Taxation Office (ATO) threshold, you can claim an offset on your tax return.
According to the ATO:
“To claim the net medical expenses tax offset in your tax return, you will need to know the total medical expenses you incurred for yourself and your dependants. You then deduct any refunds from Medicare, your health fund or any other reimbursements that relate to those expenses received during the financial year.”
Click here for updated Medicare Benefit Tax Statement information from the Department of Human Services.
Insurance
Covered If Your Policy Includes Bariatric Surgery
Insurance – Covered If Your Policy Includes Bariatric Surgery

United States: Covered If Your Plan Includes Bariatric Surgery
In the United States, if your specific policy covers bariatric surgery, gastric bypass surgery will be covered.
[insurance_new_shortcode_GS_tool]Whether your policy covers bariatric surgery depends on what kind of plan you have:
- Individual/Family Plans & Small Group Plans (through Work, under 50 employees) – The Affordable Care Act (Obamacare) requires insurance companies in many states to include coverage for bariatric surgery. Click here for an updated list of states required to cover bariatric surgery.
- Large Group Plans (through Work, 50+ employees) – Whether bariatric surgery is covered by your insurance is completely up to your company to decide. Talk with your HR department or contact your insurance company to find out if it’s covered.
- Medicare & Medicaid – Medicare and Medicaid both cover gastric bypass surgery, although not all surgeons accept them.
Click the links below for more information:
If Your Policy Covers It: Ask for Free Insurance Check
Before your insurance company will cover gastric bypass, it will require you to submit documentation from your doctor or surgeon confirming that a medically supervised weight loss program was unsuccessful.
Many surgeons offer a free insurance check and have a staff that is highly trained and experienced at working with insurance companies. Rather than figuring it out on our own, talk with a surgeon’s office about doing the legwork for you.
If Your Policy Does NOT Cover It: Seek Partial Coverage
You’ll most likely be able to get some of your gastric bypass expenses covered, even if bariatric surgery isn’t a covered benefit.
During our annual Weight Loss Surgery Cost Survey, several surgeons told us that as long as your doctor files the claim using a covered “CPT Code” (Current Procedural Terminology Code), your insurance company will likely cover it as long as the code used accurately reflects the treatment provided.
For example, there are many non-bariatric surgery reasons for your doctor to recommend:
- Lab work
- Psychological exam
- Cardiology exam
- Sleep study
- Medically supervised diet program
Each of these are also essential steps required before your surgeon will perform your surgery.
If your surgeon or primary care physician submits the above claims using a weight loss surgery CPT code, your insurance is unlikely to cover it. However, if your doctor submits the above claims using a NON-weight loss surgery CPT code, the claims will likely be considered covered benefits.
These tests will be beneficial regardless of whether you move forward with surgery, so your insurance company should have no problem covering them.
The U.S. Insurance Approval Process
The entire gastric bypass insurance approval process can take anywhere from 1 to 12 months, depending on your situation
Following are the typical steps:
- Your minimum body mass index (BMI) requirements are confirmed by your physician:
- BMI over 40 –OR–
- BMI over 35 with one or more of the following:
- Clinically significant obstructive sleep apnea
- Coronary heart disease
- Medically refractory hypertension
- Type 2 diabetes mellitus
- Other obesity-related health issues
- Complete 3 to 7 consecutive months of a medically supervised diet program, depending on your insurance company (can be coordinated by your bariatric surgeon).
- Schedule a consultation with your bariatric surgeon.
- Schedule a consultation with your primary care physician to obtain a medical clearance letter.
- Schedule a psychiatric evaluation to obtain a mental health clearance letter (usually coordinated by your bariatric surgeon).
- Schedule a nutritional evaluation from a Registered Dietitian (usually coordinated by your bariatric surgeon).
- Send all of the above documentation to your insurance company along with a detailed history of your obesity-related health problems, difficulties and treatment attempts. The review process typically happens in under one month (usually coordinated by your bariatric surgeon).
- Insurance company sends approval or denial letter:
- If approved, your surgeon’s bariatric coordinator will contact you for scheduling.
- If denied, you can choose to appeal the denial.
Your surgeon’s office will do most of this leg-work for you. They will be highly experienced in managing the process and may even have all of the required personnel on staff (e.g. registered dietitian, psychiatrist, bariatric coordinator, etc.).
Click here to access the weight loss surgeon directory to get started. Most offices will check your insurance for free to confirm coverage criteria.
For more information about gastric sleeve insurance, see our Bariatric Surgery Insurance Compete Patient Guide.
Disability Insurance During Recovery
Disability insurance (DI) is usually only available through an employer, although you can continue coverage as an individual if you leave the company.
It pays you a percentage of your monthly income if you are unable to work. Short term disability insurance (STD) most commonly pays 66 2/3% of your salary for the first 90 or 180 days of disability or sickness (also known as your disability period for bariatric surgery recovery).
Disability insurance usually includes pre-existing conditions limitations. In other words, insurance companies won’t let you buy coverage one month and go out on disability the next for something that you knew about before you signed up.
The best way to get around this for bariatric surgery is to enroll with your employer during the initial enrollment period (i.e., when you’re hired). You may not be allowed to enroll at any other time.
You must then remain enrolled for the entire “pre-existing conditions exclusionary period,” which usually lasts between 6 and 12 months. Call your insurance company, talk with HR or review your plan documents for details.
Canada: Covered, But Long Wait Times
Gastric bypass surgery is currently covered in the following provinces:
- Alberta
- British Columbia
- Manitoba
- Newfoundland and Labrador
- Nova Scotia
- Ontario
- Quebec
- Saskatchewan
Wait times range from 2 years to over 10 years, leading two out of every 3 patients to use private-pay clinics instead of public facilities.1
See our Weight Loss Surgery in Canada Patient Guide for more information.
Click here to find a private-pay clinic in Canada or the United States.
Australia: Covered by Medicare & Private Insurance
Australian Medicare will provide some reimbursement for gastric bypass surgery, although the rebate amount will still leave the majority of costs up to you and your private insurance.
To determine your rebate amount, Medicare applies a set rate to each covered procedure (that is much lower than the actual surgery costs), then they give you a rebate of 75% of that set rate.
For example, if the total procedure costs $10,000 but Medicare’s set rate is $850, then Medicare will pay $637.50 of the total bill (850 X 0.75), and you and your private insurance will be responsible for the balance.
Click here to access the Medicare Benefits Schedule (MBS) database and type in Gastric Bypass Item Number 31572 for current reimbursement levels.
Private insurance in Australia usually covers bariatric surgery, although you will still have out of pocket fees (between $1,700 and $5,300 after Medicare rebates).
Since obesity is considered a pre-existing condition, you will probably have to wait 12 months between joining a health fund and getting approved for surgery.
To get the specific coverage information and your out of pocket costs from your health fund, contact them directly and provide them with the same Medicare Item Number: 31575.
Click here for a full list of Australian health funds and their contact information.
Click here to find a top bariatric surgeon in Australia or here for our Australia Patient Guide.
Procedure
Laparoscopic, Creates Small Stomach Pouch, & Reroutes Small Intestine
Procedure – Laparoscopic, Creates Small Stomach Pouch, & Reroutes Small Intestine
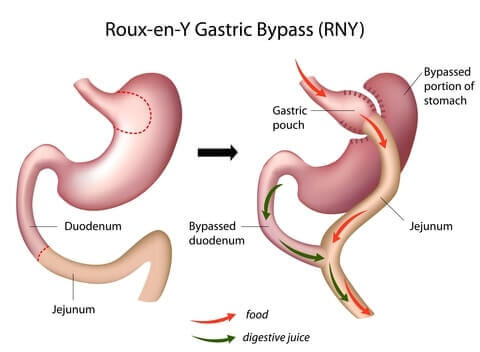
Why Gastric Bypass Works
- Reduced stomach size makes the patient feel full sooner after eating
- Rearranged intestines causes the body to absorb fewer minerals
- Dumping syndrome symptoms deter patients from eating unhealthy foods
Preparing for Surgery
During the weeks leading up to gastric bypass surgery, your surgeon’s team will do the following:
- Pre-procedure health assessment, where you will be asked questions about your medical history, medications, and surgical history
- Order certain tests like an ECG, x-ray, and blood tests
- Establish a pre-surgery diet regimen, including:
- 2 Weeks Before
- No sugar
- Lower carbs
- Increased protein
- Increased veggies
- Plenty of fluids
- 2 Days Before
- Clear liquids, broth, one protein shake per day only
- Talk with your surgeon about whether you should stop taking any medications
- 2 Hours Before
- No food or drink, no tobacco
- 2 Weeks Before
Losing as much weight as possible prior to surgery is also critical because:
- The more weight you lose pre-op, the more weight you will lose after surgery
- The lower your pre-op weight, the lower your risk of complications
- Gastric bypass surgery will not work over the long-term if you slip back into old habits. For about 70% of gastric bypass patients, eating unhealthy foods also lead to vomiting, diarrhea and other uncomfortable symptoms (37). The sooner you can start establishing good diet and exercise habits, the more likely you will be to maintain them after surgery
See our Preparing for Weight Loss Surgery page for more information.
How It’s Performed
The laparoscopic Roux-en-Y gastric bypass procedure takes about 4 hours to complete. Most patients remain in the hospital for 2 to 3 days following surgery.
The procedure serves 2 functions: it limits how much you can eat before feeling full (“restrictive”) and it prevents your body from absorbing as much food (“malabsorptive”).
Following are the steps your surgeon will perform:
- Cut and staple the stomach to create a small pouch at the end of the esophagus. Your stomach pouch will be about the size of a golf ball and hold around one ounce (28 grams) of food.
- Leave the remainder of the stomach attached to the top of the small intestines
- Go further down the small intestine, cut it, and attach it to the pouch. The food will now bypass the remainder of the stomach and top part of the small intestine.
- Take the end of the small intestine that is still connected with the remainder of the stomach and attaches it to the bottom of the “ Roux limb” of the small intestine. This allows the digestive juices produced by the stomach to meet up with the food in the intestines.
During the procedure, there will be 2 catheters (tubes) used to keep both portions of your stomach clear:
- The first is inserted through your mouth and into the pouch.
- The second is for the larger portion of the stomach and is threaded through an opening in the side of your abdomen.
Take a look at the following two videos for a more in-depth understanding…
Recovery
2 – 3 Days in Hospital, Back to Work in 2 Weeks, 4 – 6 Weeks to Full Recovery
Recovery – 2 – 3 Days in Hospital, Back to Work in 2 Weeks, 4 – 6 Weeks to Full Recovery

Gastric bypass patients usually spend 2 to 3 days in the hospital, and most patients have fully recovered in 4 to 6 weeks. Here’s what to expect following surgery:
You’ll be sore and a feel a little “out of it.” You’ll be on medication to control the pain and will likely have a bedside button to deliver additional pain meds through your IV as needed. To prevent gastrointestinal leaks, the two catheters inserted during surgery will remain in place for a couple of days to keep the stomach fluids drained.
Your surgeon will have you up and walking around as soon as possible – usually within 5 or 6 hours – to reduce the risk of blood clots and jump-start your body’s healing process. You may also be asked to wear compression stockings, use a pneumatic compression device that keeps the blood flowing in your legs, or receive blood thinners. Continue to walk as much as possible, increasing it a little each day.
Before releasing you, your surgical team will run a number of tests to ensure:
- No staple line leaks
- Wounds are healing properly
- You’re able to “pass gass”, indicating that your digestion is working properly
Fever, no improvement or worsening of pain, signs of incision infection (pus, swelling, heat, or redness), difficulty swallowing, and ongoing nausea or vomiting are all a concern. Call your surgeon immediately if any of these happen.
Your smaller stomach pouch will be sensitive, especially at first, so you’ll be on a liquid diet for a couple of weeks before slowly transitioning back to solid foods (read more about this in the Diet section of this page). Since you’ll be eating less, you may feel tired and lethargic until your body adjusts.
Your surgeon will prescribe pain and digestion medication as needed and may adjust your pre-surgery medications until you’re fully healed. Follow their instructions to the letter.
7. Return to Your “New Normal” Life
Avoid swimming or bathing until your incisions have fully healed. Many patients return to normal life and work within a couple of weeks, but plan for up to 4 to 6 weeks off to be on the safe side. Full exercise and heavy lifting typically resume within one to two months. Due to your smaller walnut-sized stomach, you will feel full much sooner than you did before surgery. To avoid stretching your new stomach pouch which can lead to weight regain, do not overeat.
8. Have Follow-Up Visits During First Year
Follow-ups with your surgeon’s team will happen about one week post-op, then 4 weeks post-op, then every 3 or 4 months to ensure that everything is on track, including:
- Discuss weight loss
- Encourage regular exercise
- Obtain lab work and make necessary adjustments to medications and dietary supplements
- Understand diet and identify any potential eating disorders
- Determine whether any potential complications may be arising
- Monitor status of obesity-related health issues
- Involve your family physician to help evaluate progress and ensure a successful transition
9. Transition to Semi-Annual or Yearly Follow-Up Visits
After you’ve reached your “low point” weight, your surgeon will probably still want to see you at least once per year (38). During those visits you may meet with several team members, including your surgeon, dietitian, and mental health care provider. They will probably request lab work to ensure that vitamin levels and other indicators are where they should be. If you experience any issues in between visits, don’t wait for your next visit… call your doctor right away.
Diet & Life After – Restricted Diet, Less Hungry, Full Sooner, Lifelong Supplements, Regular Exercise, Changing Relationships
Gastric bypass leads to impressive weight loss and health improvement, but what will day-to-day life be like? What are the tradeoffs?
Your surgery is only a tool, and long-term success requires diligence and sometimes difficult change in other areas.
Following is what to expect…
Food & Drink: Significant Changes
Following surgery, it will take about 6 weeks to transition into your new long-term gastric bypass diet which includes significant restrictions.
Timeframe Range |
2+ Weeks Before Surgery |
Recovering from surgery has its own set of challenges. Do not wait until after surgery to start your new life. Establish the following long-term diet habits ahead of time to:
Long-Term Habits to Begin Before Surgery Food
Drinks
Other Habits
|
2 Weeks Before Surgery |
You will be on a special diet 2 weeks before surgery to reduce the risk of complications. Add the following to the full ‘2+ Weeks Before’ list above:
The typical 2 week pre-op meal plan includes:
The purpose of this diet is to:
Click the buttons below for more information: |
1 Week Before Surgery |
Your surgeon will ask you to stop taking several medications one week before surgery, such as:
Avoiding these medications will reduce the risk of bleeding and stomach problems after surgery. Consult with your doctor or pharmacist prior to stopping or changing any of your medications. |
2 Days Before Surgery |
You should stop eating all foods and drink only clear liquids during the 2 days before surgery. This will clear out your digestive system before surgery. Clear liquids options include:
Do NOT consume…
|
Midnight Before Surgery to 7 Days After Surgery (Varies by Surgeon) |
Your digestive system must be completely free of food or liquids during surgery. This will reduce the risk of breathing in stomach-contents which can cause all sorts of problems like serious infection or pneumonia. A clean digestive system is especially important for patients with gastroesophageal reflux disease (GERD) or gastric paresis (paralysis of the stomach). (39) When you brush your teeth before heading to the hospital, rinse and spit out the water (don’t swallow). |
In Hospital (1 -2 Days) thru Day 7 After Surgery |
You will transition into drinking “richer” clear liquids along with the following guidelines:
Drinks that your nurse will provide may include:
Your stomach is in healing mode, so go easy on it when you return from the hospital. Be sure to drink plenty of fluids, but don’t drink too fast. Maintain the same clear liquids only diet that you were on in the hospital. Take all vitamins and supplements recommended by your surgeon. If you have no nausea or vomiting, your surgeon may allow you to try thicker items ahead of schedule (see below). Other Habits
|
Day 1 to Week 2 After Surgery (Varies by Surgeon) |
Your healing should be well underway. It’s now time to introduce thicker drinks and pureed foods. As soon as you’re ready, your surgeon will start you on many small “meals” per day which may include:
Remember: No soft or solid food and no drinks with chunks or seeds. You can also drink clear liquids between meals. While drinking anything:
|
Day 2 to Week 3 After Surgery (Varies by Surgeon) |
By this point it should be safe to add softer solids to your diet, but take it slow! When you’re ready to start pureed foods, blend water, skim milk, broth, or sugar-free juice with one of the following:
As soon as the pureed foods are going down without a problem, work your way into soft foods like:
And remember those habits you formed in the weeks and months leading up to surgery? Here’s where they start to come in handy. General diet guidelines during this stage include: Food
Drinks
Other Habits
|
Day 3 to Weeks 4+ After Surgery (Varies by Surgeon) |
Complete your slow transition to your “new normal” long-term diet. Your focus should be on eating your proteins first, in solid form (not protein shakes). Here’s why:
Other points to consider, besides those reviewed in Day 2 to Week 3 above, include:
|
Diet Requirements Timeframe Range – Diet Requirements |
2+ Weeks Before Surgery – Practice your post-bypass diet |
Recovering from surgery has its own set of challenges. Do not wait until after surgery to start your new life. Establish the following long-term diet habits ahead of time to:
Long-Term Habits to Begin Before Surgery Food
Drinks
Other Habits
|
2 Weeks Before Surgery – High protein, low sugar, low carbs |
You will be on a special diet 2 weeks before surgery to reduce the risk of complications. Add the following to the full ‘2+ Weeks Before’ list above:
The typical 2 week pre-op meal plan includes:
The purpose of this diet is to:
Click the buttons below for more information: |
1 Week Before Surgery – Stop or change some medications |
Your surgeon will ask you to stop taking several medications one week before surgery, such as:
Avoiding these medications will reduce the risk of bleeding and stomach problems after surgery. Consult with your doctor or pharmacist prior to stopping or changing any of your medications. |
2 Days Before Surgery – Clear liquids only |
You should stop eating all foods and drink only clear liquids during the 2 days before surgery. This will clear out your digestive system before surgery. Clear liquids options include:
Do NOT consume…
|
Midnight Before Surgery to 7 Days After Surgery (Varies by Surgeon) – Nothing to eat or drink |
Your digestive system must be completely free of food or liquids during surgery. This will reduce the risk of breathing in stomach-contents which can cause all sorts of problems like serious infection or pneumonia. A clean digestive system is especially important for patients with gastroesophageal reflux disease (GERD) or gastric paresis (paralysis of the stomach). (31) When you brush your teeth before heading to the hospital, rinse and spit out the water (don’t swallow). |
In Hospital (1 -2 Days) thru Day 7 After Surgery Clear liquids only |
You will transition into drinking “richer” clear liquids along with the following guidelines:
Drinks that your nurse will provide may include:
Your stomach is in healing mode, so go easy on it when you return from the hospital. Be sure to drink plenty of fluids, but don’t drink too fast. Maintain the same clear liquids only diet that you were on in the hospital. Take all vitamins and supplements recommended by your surgeon. If you have no nausea or vomiting, your surgeon may allow you to try thicker items ahead of schedule (see below). Other Habits
|
Week 2 After Surgery – Add thicker drinks & smooth foods (no chunks) |
Your healing should be well underway. It’s now time to introduce thicker drinks and pureed foods. As soon as you’re ready, your surgeon will start you on many small “meals” per day which may include:
Remember: No soft or solid food and no drinks with chunks or seeds. You can also drink clear liquids between meals. While drinking anything:
|
Week 3 After Surgery – Slowly test pureed & soft solid foods |
By this point it should be safe to add softer solids to your diet, but take it slow! When you’re ready to start pureed foods, blend water, skim milk, broth, or sugar-free juice with one of the following:
As soon as the pureed foods are going down without a problem, work your way into soft foods like:
And remember those habits you formed in the weeks and months leading up to surgery? Here’s where they start to come in handy. General diet guidelines during this stage include: Food
Drinks
Other Habits
|
Day 3 to Weeks 4+ After Surgery (Varies by Surgeon) Slowly test solid foods |
Complete your slow transition to your “new normal” long-term diet. Your focus should be on eating your proteins first, in solid form (not protein shakes). Here’s why:
Other points to consider, besides those reviewed in Day 2 to Week 3 above, include:
|
For more information, see our Bariatric Diet page.
Vitamins & Supplements: Lifelong & Crucial
Since gastric bypass is a “malabsorptive” procedure by nature, it carries a high risk of malnutrition. Patients must be extremely diligent about taking prescribed vitamins and supplements or risk serious vitamin deficiency.
Vitamins |
A daily multivitamin with mineral supplements will help prevent hair loss and general nutrition problems.
|
Calcium (42) |
Calcium citrate supplements will keep your bones strong.
|
Folate (folic acid) (43) |
Patients who don’t get enough folate are at a higher risk of anemia.
|
Patients low on iron are more likely to have a stroke, heart attack, or other blood-related problems. Some patients may require additional iron, which should be taken with Vitamin C for better absorption. For these patients, Iron supplements must be taken forever. |
Thiamin (Vitamin B1) |
Thiamin deficiency, also called Beriberi, can result in loss of appetite, headaches, nausea, weakness, irritability, depression, abdominal discomfort, pain in the limbs, shortness of breath, and swollen feet or legs Deficiency may occur after vomiting, skipped meals, or missed supplementation |
Without enough Vitamin D, you’re at risk of developing rickets, a weakening of the bones, muscles, and teeth.
Talk with your surgeon to be sure, but you may be able to find a calcium supplement that fulfills your Vitamin D requirements. |
Vitamin B12 |
Your central nervous system relies on Vitamin B12, and not getting enough of it could lead to serious issues like numbness, memory loss or even paralysis.
|
Body Part Affected Vitamins – Body Part Affected |
A daily multivitamin with mineral supplements will help prevent hair loss and general nutrition problems.
|
Calcium nitrate supplements will keep your bones strong.
|
Patients who don’t get enough folate are at a higher risk of anemia.
|
Patients low on iron are more likely to have a stroke, heart attack, or other blood-related problems. Some patients may require additional iron, which should be taken with Vitamin C for better absorption. For these patients, Iron supplements must be taken forever. |
Thiamin (Vitamin B1) – Entire Body |
Thiamin deficiency, also called Beriberi, can result in loss of appetite, headaches, nausea, weakness, irritability, depression, abdominal discomfort, pain in the limbs, shortness of breath, and swollen feet or legs. Deficiency may occur after vomiting, skipped meals, or missed supplementation |
Without enough Vitamin D, you’re at risk of developing rickets, a weakening of the bones, muscles, and teeth.
Talk with your surgeon to be sure, but you may be able to find a calcium supplement that fulfills your Vitamin D requirements. |
Vitamin B12 – Brain/Nervous System |
Your central nervous system relies on Vitamin B12, and not getting enough of it could lead to serious issues like numbness, memory loss or even paralysis.
|
For more information, see our Bariatric Vitamins page.
Exercise: 2.5 hours per week, spread out over 2 to 4 days

Exercise is almost as important as what you eat after gastric bypass surgery for two big reasons:
- Patients who exercise regularly lose more weight over the long-term
- Physical and mental health benefits make you much more likely to keep your new lifestyle requirements in line
How much exercise do you need to for noticeable results?
One study found that exercising 2.5 hours per week leads to 5.7% more weight loss (50). Another showed that gastric bypass patients who exercise at least 30 minutes a day, 3 days per week have a 4+% lower body mass index (51).
Further, regular exercise leads to quicker improvement in obesity-related health problems following surgery (52).
To help you stay on track:
- Block out time to exercise at the same times on the same days of the week.
- Spread your workouts over 3 or 4 days each week rather than having one or two long sessions. In addition to building endurance, this will make working out less intimidating.
Exercise Types
When choosing your exercise routine, focus on three aspects: endurance, flexibility, and strength. Here are suggestions for each:
- Endurance:
- Walking
- Stationary bike
- Swimming (best option)
- Flexibility
- Well-rounded stretching routine, ideally yoga since it incorporates proper breathing and uses your own bodyweight to build strength
- Strength
- Exercise balls
- Weights
- Yoga
See our Exercise After Bariatric Surgery page for more information.
Your Brain: Less Hungry, Careful About Food Addiction, New Mentality Will Change Behavior & Relationships
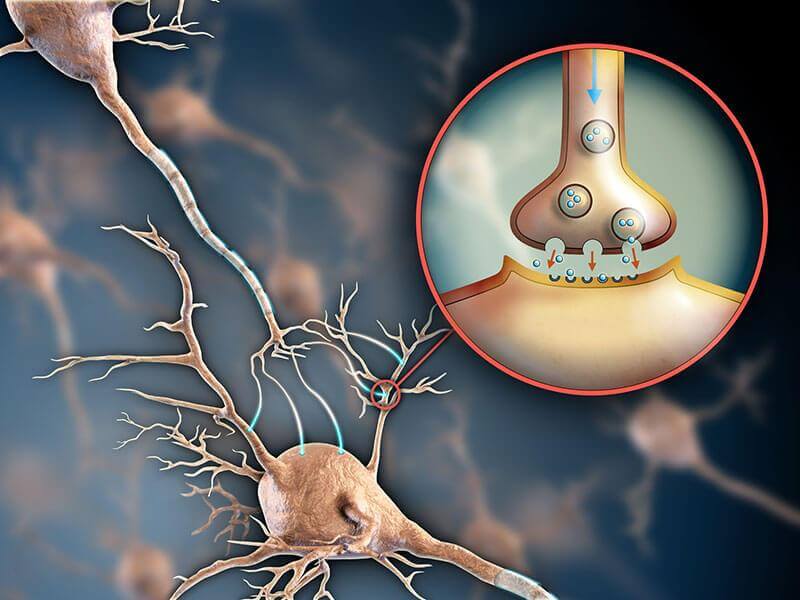
Ghrelin Hormone & Hunger
The big diet changes reviewed above may be easier than they sound for two reasons:
- You may permanently feel less hungry following surgery since the production of a key hunger-causing hormone, ghrelin, will be reduced
- Your stomach will be much smaller, causing you to feel full much sooner after eating
Food Addiction
If not addressed prior to surgery, food addiction can lead to long-term weight regain for gastric bypass patients. If you struggle with food addiction, talk with your surgeon before moving forward with surgery.
To find out if you may be suffering from food addiction, take our Food Addiction Quiz.
Relationships After Weight Loss

Gastric bypass leads to rapid and significant weight loss, and people will start treating you differently within a couple of months after surgery. Following are positive experiences reported by most patients:
- Treated with more respect
- More romantic interest from others
- No more obesity discrimination
- Deeper relationships as a result of being able to physically keep up with kids and more physically fit friends
- More compliments from others
- Increased self-confidence
However, being “newly thin” may carry unforeseen negatives as well:
- How will overweight friends or family members feel when you’re losing weight but they are not?
- If they’re not making diet and lifestyle changes as well, will your friends or family make it more difficult for you to stay on track?
- How will your coworkers react? Should you even tell them you are having surgery?
- Will your new healthier diet and smaller portion sizes make meals with others awkward?
- Could intimacy with your spouse or partner be effected?
- Could your spouse or partner become jealous now that others are noticing you more?
The way you view people and relationships may change as well. Common thoughts include:
- “Would this person be treating me the same way if I hadn’t lost all of this weight?”
- “How do I handle obesity discrimination now that I’m on the “other side”?”
For real life experiences and advice from other gastric bypass patients, see our Relationships After Weight Loss surgery page.
Downsides
Risk of Complications, Side Effects, & Weight Regain
Downsides – Risk of Complications, Side Effects, & Weight Regain

Like all bariatric surgery procedures, mortality rates for gastric bypass (risk of dying) are extremely low. It has a survival rate of 998 out of every 1,000 patients.
However, complications are more common, with about to 1 out of 7 patients experiencing one or more over the long-term (53, 54).
Preventing Gastric Bypass Complications
Follow these steps to reduce your risk of gastric bypass complications:
- Select the surgery that is most appropriate for your situation. Different surgeries carry different risks for different people. Our Types of Bariatric Surgery page compares and contrasts the safest and most effective procedures.
- Choose an experienced surgeon, since more experienced surgeons tend to have better outcomes. For example, one study evaluated a surgeon over his first 300 laparoscopic gastric bypass patients. Following were his results as he gained experience (55):GroupGroupFirst 100 patientsFirst 100 patientsSecond 100 patientsSecond 100 patientsThird 100 patientsThird 100 patientsGroupTime in surgeryFirst 100 patients163 minutesSecond 100 patients119 minutesThird 100 patients94 minutesGroupNumber of reoperationsFirst 100 patients9Second 100 patients2Third 100 patients1GroupNumber of conversions to open surgeryFirst 100 patients2Second 100 patients1Third 100 patients1
As you can see, the more procedures he performed, the lower the time it took to perform the surgery and the lower the number of reoperations required.
A separate and much larger study of over 15,000 patients in Michigan had similar findings (56):
# of procedures performed by surgeon over 3 years# of procedures performed by surgeon over 3 yearsLess than 100 casesLess than 100 cases100 – 249 cases100 – 249 casesGreater than or equal to 250 casesGreater than or equal to 250 cases# of procedures performed by surgeon over 3 yearsRate of serious complications occuring within 30 days of surgeryLess than 100 cases3.8%100 – 249 cases2.4%Greater than or equal to 250 cases1.9%Most surgeons offer free seminars that teach you about your weight loss surgery options, their practice’s experience, total procedures performed, and specific results. The seminars also allow you to get to know the surgeon prior to a one-on-one consultation.
You can also review our Bariatric Doctors page to learn how to interview multiple doctors and choose the best one.
- Eat and exercise as directed by your surgeon before, during, and after surgery. Your behavior before and after surgery directly and significantly impacts your gastric bypass complication risk. Read the other sections of this page for more information.
Possible Gastric Bypass Complications
The most common complications, which occur in greater than 1% of patients, include (57):
Stomal Stenosis – About 5% of patients
Wound Infection – About 3% of patients
Bowel Obstruction – About 3% of patients
Leak – About 2% of patients
Gastrointestinal bleeding – About 2% of patients
For a full list of potential issues, see our Gastric Bypass Complications page.
Gastric Bypass Side Effects: Digestion/Diet Issues, Dental Problems, Sagging Skin, & Others
Click below for more information about each gastric bypass side effect:
Digestion & Diet Issues
- Dumping syndrome is experienced by 7 out of 10 gastric bypass patients, although for 95% of these patients, symptoms are relatively minor (59). Symptoms may include weakness, dizziness, flushing and warmth, nausea and palpitation immediately or shortly after eating. They are caused by abnormally rapid emptying of the stomach especially in individuals who have had part of the stomach removed.
While this sounds like a bad thing, many patients view it as a “blessing in disguise.” The symptoms of dumping syndrome are completely avoidable by eating a proper bariatric diet… can you think of a more convincing way to keep you on track? In fact, some patients who do not suffer from dumping syndrome often comment that they wish they did, as “dumping” removes some of the choice involved in food selections. See our Dumping Syndrome page for more details.
- Dehydration – an abnormal depletion of body fluids. You will need to drink a lot of water in the months following surgery – as much as 2 liters per day. Not doing so can lead to nausea and vomiting which can lead to even worse dehydration and other problems. In severe cases of dehydration patients may need to return to the hospital for IV fluids and vitamins.
- Difficulty swallowing (also called dysphagia) can be caused by eating too quickly, too much or not chewing food enough and can usually be fixed by avoiding these issues.
- Indigestion (also called dyspepsia) is the inability to digest or difficulty in digesting food, the incomplete or imperfect digestion of food or a case or attack of indigestion marked especially by a burning sensation or discomfort in the upper abdomen.
Treatment is usually as simple as changing your diet, such as avoiding greasy foods or limiting liquid intake to certain times of day. Alcohol, aspirin and other drugs are also causes. If diet changes don’t work, antacids and H2 blockers are sometimes prescribed.
- Intolerance to certain foods, beverages and drugs – With a changed stomach size and digestive system, there will be certain foods, beverages and drugs that you’ll need to avoid and certain diet habits you’ll need to maintain.It is important to talk with your doctor before taking ANY drugs, as they can damage your stomach pouch after gastric bypass surgery and cause ulcers (including over the counter pain relievers – Motrin, Advil, aspirin, Aleve).
Regarding alcohol, a little may still be okay, but it will have a profoundly different effect on your body than it used to. First, it’s bad for your diet due to the large amounts of calories found in many alcoholic beverages. Second, you will become intoxicated more quickly following surgery which could lead to a number of problems.
Finally, following surgery the effects of alcohol on your system could make liver disease more likely. As for smokers, you must stop now. If you smoke after gastric bypass surgery, there is a good chance that you will get an ulcer in your pouch.
- Nausea and vomiting is one of the most common gastric bypass side effects and is experienced in up to 70% of patients. Following your doctor’s bariatric diet recommendations exactly will typically fix or improve the problem. While in the hospital, receiving a larger amount of IV fluids at a faster rate may make you less likely to feel nauseous or vomit (60). Keeping a food journal for a couple of days may help you to pinpoint the foods which seem to cause nausea and vomiting.
- Change in bowel habits – bowel function after bariatric surgery may change in a number of ways, including (61)…
- Diarrhea or loose stools – usually completely dependent on diet – you will need to figure out and avoid foods that “trigger” diarrhea. It could also be the result of lactose intolerance (not a side effect of surgery, but surgery can make you more sensitive to a problem that you didn’t know you had) which would require dairy products to be removed from the diet.
- Constipation – usually fixed by increasing the amount of water you are drinking and by taking fiber supplements.
Dental Problems
Some gastric bypass patients experience problems with their teeth after surgery due to:
- Malabsorption
- Not taking proper vitamins in the right amounts
- Potential pH changes in the saliva after surgery
- Poor dental hygiene
- Not addressing significant reflux or vomiting issues (stomach acid in the mouth is bad for the teeth)
See our Dental Problems After Gastric Bypass Surgery page for a dialogue between several patients, dentists and bariatric surgeons about the issue.
Sagging Skin
Gastric bypass surgery causes most patients to lose weight fast, and your skin simply can’t keep up.
Sagging skin can cause several mental and physical issues including:
- Difficulty getting dressed
- Difficulty exercising, which may impact long-term weight maintenance and health
- Embarrassment with or without clothes on
- Skin fold rashes or breakdown of skin
- Skin fold infections
Options for addressing sagging skin include:
- Body-contouring undergarments
- Plastic surgery to remove the excess skin, which is often covered by insurance. See our Plastic Surgery After Weight Loss page for more information.
Other Potential Side Effects
- Gallstones are small stones of cholesterol formed in the gallbladder or bile passages. They can be created following rapid weight loss which leads to their development in as many as 1/3 of bariatric surgery patients. To prevent this, your surgeon may remove your gallbladder during surgery or prescribe bile salt supplements after surgery.
- Hair Loss occurs to some degree for most patients and can be caused by nutritional deficiencies or as your body’s response to major surgery or extreme weight loss. Most patients stop losing and start regrowing hair within 3 to 6 months following surgery. Supplementing your diet with protein, vitamin B, magnesium, calcium and zinc, among other bariatric vitamins, will help prevent hair loss and improve hair growth.
- Kidney stones are stones in the kidney related to decreased urine volume or increased excretion of stone-forming components such as calcium, oxalate, urate, cystine, xanthine and phosphate. The stones form in the urine collecting area (the pelvis) of the kidney and may range in size from tiny to staghorn stones the size of the renal pelvis itself. Drinking lots of water, which gastric bypass patients should do anyway, will help to dilute the urine and may help prevent kidney stones.
Weight Regain: Half of All Bypass Patients After 2 Years
About half of all gastric bypass patients start to regain weight after two years.
After five years, the average bypass patient gains back about 8% of their weight compared to their 18-month to 2-year “low point.” (62)
Another study found that that up to 20% of morbidly obese patients (40 – 50 BMI) and up to 35% of super obese patients (BMI over 50) gained back more than 50% of their excess weight after 10 years (63).
Equally concerning, the more weight you gain back, the more likely your health problems are to come back. For example, one study showed that after gastric bypass surgery, all patients with Type 2 Diabetes experienced improvement or complete resolution. However, after 3 years, about 1 out of 4 of those patients saw their diabetes worsen or come back (64).
Why do patients gain back weight?
Usually it’s the patient’s fault. They veer off course and consume foods or beverages they shouldn’t, causing their stomach pouch or the connection between their stomach and small intestines (called the “stoma”) to stretch out (65).
If you start to gain back weight, contact your surgeon or dietitian immediately to assess your diet and exercise habits.
See our Weight Regain After Bariatric Surgery page for advice on how to avoid weight regain after gastric bypass surgery.
See the Revision section below for options to surgically address weight regain.
Revision
4 Surgical Options to Address Weight Regain
Revision – 4 Surgical Options to Address Weight Regain
Gastric bypass revision surgery may be an option in the following two circumstances:
- Stretched stomach – reducing the size of a stretched stomach will cause your stomach to hold less, making you feel full sooner, just like after surgery.
- Stretched stoma (connection between stomach and small intestine) – a properly sized stoma will cause your stomach to drain more slowly, prolonging your feelings of fullness.
In these cases, your surgeon will most likely choose one of the following procedures:
- Shrink the stoma by injecting a sclerosant. The injections attempt to create scarring that reduce the size of the stoma (connection between the stomach and small intestines).
- Add adjustable gastric band (convert to lap band surgery)
- Lengthen Roux limb – this somewhat controversial procedure is usually only considered when the patient has a very low base metabolic rate and continues with poor weight loss results despite an augmented exercise program.
- Convert to duodenal switch – more likely to be recommended by your surgeon if you were considered “super obese” (BMI over 50) prior to your initial surgery.
See our Gastric Bypass Revision page for more information.
Vs Other Types of Surgery – Similar or Better Weight Loss & Health Improvement, Similar or Higher Risk of Complications & Side Effects

Gastric bypass was considered the “gold standard” procedure for several years, until gastric sleeve surgery took its place.
However, it is still recommended by surgeons for some patients for its unique combination of benefits.
Picture of Procedure (click to expand) Picture of Procedure (click to expand) |
Video of Procedure Video of Procedure |
External Device Placed Inside Body? External Device Placed Inside Body? |
Year Device/Product Approved Year Device/ Product Approved |
Average Total Cost Before Insurance (U.S.) Average Total Cost Before Insurance (U.S.) |
Covered by Insurance? Covered by Insurance? |
Financing Available? Financing Available? |
BMI Requirements BMI Requirements |
Avg % Excess Weight Loss After 5 Years Avg % Excess Weight Loss After 5 Years |
Health Improvement Health Improvement |
Procedure Type Procedure Type |
Complication Rate Complication Rate |
Mortality Rate Mortality Rate |
Reversible? Reversible? |
Time Until Removed Time Until Removed |
Alters Path of Digestion (Higher Risk of Mal-absorption)? Alters Path of Digestion (Higher Risk of Mal-absorption)? |
Procedure Time (Average) Procedure Time (Average) |
Hospital Stay (Average) Hospital Stay (Average) |
Recovery Time (Back to Work) – Average Recovery Time (Back to Work) – Average |
Diet Challenges (Procedure-Specific; Click here for general diet changes to expect) Diet Challenges (Procedure-Specific; Click here for general diet changes to expect) |
Food Cravings Likely to Decrease? Food Cravings Likely to Decrease? |
Difficulty Swallowing? (due to food backing up because of smaller stomach) Difficulty Swallowing? (due to food backing up because of smaller stomach) |
Digestion & Bowel Movement Post-Recovery (Relatively common issues) Digestion & Bowel Movement Post-Recovery (Relatively common issues) |
Qualified Surgeons Qualified Surgeons |
Patient Guides Patient Guides |
Gastric Bypass |
Picture of Procedure (click to expand) |
External Device Placed Inside Body? No |
Year Device/Product Approved n/a |
Average Total Cost Before Insurance (U.S.) $24,000 |
Covered by Insurance? Yes (other than some individual policies) |
Financing Available? Yes |
BMI Requirements 35 – 39.9 with health problems; 40+ without |
Avg % Excess Weight Loss After 5 Years 50 – 70% |
Health Improvement Compare % excess weight loss; the more weight loss, the more health improvement
|
Procedure Type Laparoscopic |
Complication Rate Up to 15% |
Mortality Rate 0.24% |
Reversible? No |
Time Until Removed n/a |
Alters Path of Digestion (Higher Risk of Malabsorption)? Yes |
Procedure Time (Average) ~4 hours |
Hospital Stay (Average) 2 to 3 days |
Recovery Time (Back to Work) – Average ~2 weeks |
Diet Challenges (Procedure-Specific; Click here for general diet changes to expect) Potential problem foods:Sugars, Refined fats, Carbs, Dairy. Malabsorption will require life-long vitamin supple-mentation. |
Food Cravings Likely to Decrease? Maybe |
Difficulty Swallowing? (due to food backing up because of smaller stomach) Possible |
Digestion & Bowel Movement Post-Recovery (Relatively common issues) Dumping syndrome occurs in ~80% of patients who eat sugar, refined fats, or carbs. |
Qualified Surgeons Broad Network – Click Here to Find Surgeon |
Patient Guides (this page) |
Gastric Sleeve |
Picture of Procedure (click to expand) |
External Device Placed Inside Body? No |
Year Device/Product Approved n/a |
Average Total Cost Before Insurance (U.S.) $19,000 |
Covered by Insurance? Yes (other than some individual policies) |
Financing Available? Yes |
BMI Requirements 35 – 39.9 with health problems; 40+ without |
Avg % Excess Weight Loss After 5 Years 64 – 75% |
Health Improvement Compare % excess weight loss; the more weight loss, the more health improvement |
Procedure Type Laparoscopic |
Complication Rate Up to 10% |
Mortality Rate 0.19% |
Reversible? No |
Time Until Removed n/a |
Alters Path of Digestion (Higher Risk of Malabsorption)? No |
Procedure Time (Average) ~2 hours |
Hospital Stay (Average) 2 to 3 days |
Recovery Time (Back to Work) – Average ~2 weeks |
Diet Challenges (Procedure-Specific; Click here for general diet changes to expect) Potential problem foods: Dairy |
Food Cravings Likely to Decrease? Maybe |
Difficulty Swallowing? (due to food backing up because of smaller stomach) Possible |
Digestion & Bowel Movement Post-Recovery (Relatively common issues) GERD (reflux) in ~1 out of 5 patients after 1 year, drops to 1~ out of 33 patients after 3 year.
Some patients experience diarrhea. |
Qualified Surgeons Broad Network – Click Here to Find Surgeon |
Patient Guides |
Lap Band |
Picture of Procedure (click to expand) |
External Device Placed Inside Body? Yes |
Year Device/Product Approved 2011 (FDA10) |
Average Total Cost Before Insurance (U.S.) $15,000 |
Covered by Insurance? Yes (other than some individual policies) |
Financing Available? Yes |
BMI Requirements 35 – 39.9 with health problems; 40+ without |
Avg % Excess Weight Loss After 5 Years 25 – 80% (extremely variable among patients) |
Health Improvement Compare % excess weight loss; the more weight loss, the more health improvement |
Procedure Type Laparoscopic |
Complication Rate Up to 33% |
Mortality Rate 0.10% |
Reversible? Yes |
Time Until Removed Patient-Specific (not necessarily required) |
Alters Path of Digestion (Higher Risk of Malabsorption)? No |
Procedure Time (Average) ~1 hour |
Hospital Stay (Average) Outpatient to 1 day |
Recovery Time (Back to Work) – Average ~2 weeks |
Diet Challenges
(Procedure-Specific; Click here for general diet changes to expect) Potential problem foods: Dairy.
Should not drink anything within 30 minutes before or after eating |
Food Cravings Likely to Decrease? No |
Difficulty Swallowing? (due to food backing up because of smaller stomach) Possible |
Digestion & Bowel Movement Post-Recovery (Relatively common issues) Reflux and vomiting common if band too tight (can be adjusted).
Some patients experience constipation. |
Qualified Surgeons Broad Network – Click Here to Find Surgeon |
Patient Guides |
Duodenal Switch |
Picture of Procedure (click to expand) |
External Device Placed Inside Body? No |
Year Device/Product Approved n/a |
Average Total Cost Before Insurance (U.S.) $27,000 |
Covered by Insurance? Yes (other than some individual policies) |
Financing Available? Yes |
BMI Requirements 35 – 39.9 with health problems; 40+ without
(but more common for 50+) |
Avg % Excess Weight Loss After 5 Years 65 – 75% |
Health Improvement Compare % excess weight loss; the more weight loss, the more health improvement |
Procedure Type Laparoscopic |
Complication Rate Up to 24% |
Mortality Rate Up to 1.1% (but procedure tends to be performed on heavier patients who have higher risk) |
Reversible? No |
Time Until Removed n/a |
Alters Path of Digestion (Higher Risk of Malabsorption)? Yes |
Procedure Time (Average) 3.5 – 4.5 hours |
Hospital Stay (Average) 2 to 3 days |
Recovery Time (Back to Work) – Average ~2 weeks |
Diet Challenges(Procedure-Specific; Click here for general diet changes to expect) Malabsorption will require life-long vitamin supple-mentation. |
Food Cravings Likely to Decrease? Maybe |
Difficulty Swallowing? (due to food backing up because of smaller stomach) Possible |
Digestion & Bowel Movement Post-Recovery (Relatively common issues) Might be significant, including frequency, diarrhea, and/or foul-smelling stools/ flatulence. |
Qualified Surgeons Fewer Options – Click Here to Find Surgeon |
Patient Guides |
Gastric Balloon |
Picture of Procedure (click to expand) |
External Device Placed Inside Body? Yes |
Year Device/Product Approved 2015 (FDA11) |
Average Total Cost Before Insurance (U.S.) $8,150 |
Covered by Insurance? Possible with aggressive negotiation and appeals |
Financing Available? Yes |
BMI Requirements Between 30 & 40 in U.S. (above 27 elsewhere) |
Avg % Excess Weight Loss After 5 Years n/a (must be removed after 6 months; weight loss during that time is 26 – 46%) |
Health Improvement Compare % excess weight loss; the more weight loss, the more health improvement |
Procedure Type Through Mouth |
Complication Rate Up to 10% |
Mortality Rate Close to 0% |
Reversible? Yes |
Time Until Removed 6 months max |
Alters Path of Digestion (Higher Risk of Malabsorption)? No |
Procedure Time (Average) 30 minutes or less |
Hospital Stay (Average) Outpatient |
Recovery Time (Back to Work) – Average 3 – 4 days |
Click here for general diet changes to expect) Potential Problem Foods: Pasta and other foods that might stick to balloon in stomach. |
Food Cravings Likely to Decrease? No |
Difficulty Swallowing? (due to food backing up because of smaller stomach) Unlikely |
Digestion & Bowel Movement Post-Recovery (Relatively common issues) Vomiting possible (but often avoidable with proper habits). “Feeling bloated” reported by some patients. |
Qualified Surgeons Fewer Options – Click Here to Find Surgeon |
Patient Guides |
vBloc |
Picture of Procedure (click to expand) |
External Device Placed Inside Body? Yes |
Year Device/Product Approved 2015 (FDA9) |
Average Total Cost Before Insurance (U.S.) $18,500 |
Covered by Insurance? Possible with aggressive negotiation and appeals |
Financing Available? Yes |
BMI Requirements 35 – 39.9 with health problems; 40 – 45 without (none over 45) |
Avg % Excess Weight Loss After 5 Years 17 – 28% |
Health Improvement Compare % excess weight loss; the more weight loss, the more health improvement |
Procedure Type Laparoscopic |
Complication Rate 3 – 4% |
Mortality Rate Close to 0% |
Reversible? Yes |
Time Until Removed Patient-Specific (not necessarily required) |
Alters Path of Digestion (Higher Risk of Malabsorption)? No |
Procedure Time (Average) 60 to 90 minutes |
Hospital Stay (Average) Outpatient |
Recovery Time (Back to Work) – Average 3 – 4 days |
Diet Challenges (Procedure-Specific; Click here for general diet changes to expect) None, but healthier eating recommended for better results |
Food Cravings Likely to Decrease? Yes |
Difficulty Swallowing? (due to food backing up because of smaller stomach) No |
Digestion & Bowel Movement Post-Recovery (Relatively common issues) None |
Qualified Surgeons Fewer Options – Click Here to Find Surgeon |
Patient Guides |
Gastric Bypass Positives
- Weight loss is usually in range of gastric sleeve and much better (on average) than after Lap Band surgery, gastric balloon, or vBloc Therapy (but less than duodenal switch). The AspireAssist needs more research, but initial results show a weight loss potential less than gastric bypass.
- Health Improvement is generally better than after gastric sleeve, Lap Band, gastric balloon, or vBloc Therapy (but not as good as duodenal switch). Intital research shows AspireAssist will have similar health improvements to gastric balloon or vBloc Therapy, but more research is needed to confirm.
- Short-term risk of gastric bypass is similar to that of gastric sleeve and lower than duodenal switch (but higher than Lap Band, gastric balloon, vBloc Therapy, or AspireAssist).
- Long-term risk of gastric bypass is lower than duodenal switch (but higher than gastric sleeve, and Lap Band surgery; long-term data not yet available for balloon, vBloc, or AspireAssist).
- There is no external device left inside the body as there is with Lap Band, gastric balloon, vBloc Therapy, and AspireAssist, so there is no risk of device-related complications. While the risk of device-related complications is relatively low for vBloc Therapy, gastric balloon, and AspireAssist, it is a concern and should be considered for Lap Band.
- If you are on anticoagulation medication (blood thinners), compared with gastric sleeve, gastric bypass surgery is probably a better choice to reduce the risk of marginal ulcers.
Gastric Bypass Negatives
- Not reversible – Unlike Lap Band, gastric balloon, vBloc Therapy, and AspireAssist, gastric bypass surgery (along with gastric sleeve and duodenal switch) should be considered irreversible – once your stomach size is reduced and your intestines are rerouted, it is very it is very difficult and uncommon for the procedure to be reversed.
- Weight loss (on average) is usually lower than duodenal switch (but higher or similar to all other procedures).
- Health Improvement is generally not as significant as after duodenal switch (but is generally better than all other procedures).
- While survival rate is extremely high at 998 out of every 1,000 patients, risk of gastric bypass complications is higher than all other procedures except duodenal switch. Early complications occur in about 1 out of 10 patients while late complications occur in about 1 out of 7 (66, 67).
- The two primarily “malabsorptive” procedures, gastric bypass and duodenal switch, are more complicated to perform and include the rearranging your digestive system. As a result, they have a:
- Longer recovery
- Higher risk of vitamin deficiency (and therefore require more daily supplements)
- Higher costs
- Dumping syndrome is experienced by up to 7 out of 10 gastric bypass patients, although many patients report this being a “good thing” since it helps them keep their diet on track (see more in the Downsides section above).
Click here to review studies that directly compare gastric bypass surgery to other forms of weight loss surgery.
Summary of Findings When Comparing Gastric Bypass to Other Procedures Summary of Findings When Comparing Gastric Bypass to Other Procedures |
Lap Band Surgery vs Gastric Bypass Lap Band Surgery vs Gastric Bypass |
Roux-en-Y gastric bypass is associated with better weight loss, resulting in a better correction of some comorbidities than gastric banding, at the price of a higher early complication rate. This difference, however, is largely compensated by the much higher long-term complication and reoperation rates seen after gastric banding.O Roux-en-Y gastric bypass is associated with better weight loss, resulting in a better correction of some comorbidities than gastric banding, at the price of a higher early complication rate. This difference, however, is largely compensated by the much higher long-term complication and reoperation rates seen after gastric banding.O |
Weight loss outcomes strongly favored gastric bypass over lap band surgery. Patients treated with lap band had lower short-term morbidity than those treated with gastric bypass, but reoperation rates were higher among patients who received lap band surgery. Gastric bypass should remain the primary bariatric procedure used to treat obesity in the United States.A Editor’s Note: This study was published before long-term results had been published for gastric sleeve surgery. Weight loss outcomes strongly favored gastric bypass over lap band surgery. Patients treated withlap band had lower short-term morbidity than those treated with gastric bypass, but reoperation rates were higher among patients who receivedlap band surgery. Gastric bypass should remain the primary bariatric procedure used to treat obesity in the United States.A Editor’s Note: This study was published before long-term results had been published for gastric sleeve surgery. |
Collectively, data clearly point to distinct changes in dietary habits after bariatric operations which markedly differ between gastric bypass andlap band patients. Overall, it is tempting to conclude that gastric bypass operations lead to a healthier and a more balanced diet thanlap band implantations.B Collectively, data clearly point to distinct changes in dietary habits after bariatric operations which markedly differ between gastric bypass andlap band patients. Overall, it is tempting to conclude that gastric bypass operations lead to a healthier and a more balanced diet thanlap band implantations.B |
Gastric bypass seems to provide a stronger suppression of ghrelin in comparison with gastric lap band procedure. These findings are consistent with the hypothesis that suppression of ghrelin is one mechanism by which gastric bypass can reduce body weight long term, more thanlap band.C Gastric bypass seems to provide a stronger suppression of ghrelin in comparison with gastric lap band procedure. These findings are consistent with the hypothesis that suppression of ghrelin is one mechanism by which gastric bypass can reduce body weight long term, more thanlap band.C |
Mini Gastric Bypass Surgery vs Gastric Bypass Mini Gastric Bypass Surgery vs Gastric Bypass |
Pending long-term evaluation, mini gastric bypass surgery seems a good alternative to gastric bypass, giving the same results with a more simple and reproducible technique.D Pending long-term evaluation, mini gastric bypass surgery seems a good alternative to gastric bypass, giving the same results with a more simple and reproducible technique.D |
Previous studies have demonstrated that hospitalization after gastric bypass increases remarkably (20% per year). The present study shows that hospitalization followingmini gastric bypass surgery instead of rising, as reported with gastric bypass, decreases by a third. Themini gastric bypass has been shown to be a short, safe successful weight loss surgery in previous work. The present study supports themini gastric bypass as a low risk procedure that decreases the need for hospitalization.E Previous studies have demonstrated that hospitalization after gastric bypass increases remarkably (20% per year). The present study shows that hospitalization followingmini gastric bypass surgery instead of rising, as reported with gastric bypass, decreases by a third. Themini gastric bypass has been shown to be a short, safe successful weight loss surgery in previous work. The present study supports themini gastric bypass as a low risk procedure that decreases the need for hospitalization.E |
Both gastric bypass andmini gastric bypass surgery are effective for morbid obesity with similar results for resolution of metabolic syndrome and improvement of quality of life. Mini gastric bypass surgery is a simpler and safer procedure that has no disadvantage compared with gastric bypass at 2 years of follow-up.F Both gastric bypass andmini gastric bypass surgery are effective for morbid obesity with similar results for resolution of metabolic syndrome and improvement of quality of life. Mini gastric bypass surgery is a simpler and safer procedure that has no disadvantage compared with gastric bypass at 2 years of follow-up.F |
Gastric Sleeve Surgery vs Gastric Bypass Gastric Sleeve Surgery vs Gastric Bypass |
Compared with gastric sleeve, gastric bypass had significantly better effect in resolving type 2 diabetes mellitus, hypertension, hypercholesterolemia, gastroesophageal reflux disease, and arthritis. However, gastric bypass had higher incidence of complications and reoperation, and longer operation time than gastric sleeve.P Compared with gastric sleeve, gastric bypass had significantly better effect in resolving type 2 diabetes mellitus, hypertension, hypercholesterolemia, gastroesophageal reflux disease, and arthritis. However, gastric bypass had higher incidence of complications and reoperation, and longer operation time than gastric sleeve.P |
Overall complication rates among patients undergoing gastric sleeve (SG) (6.3%) were significantly lower than for gastric bypass (RYGB) (10.0%, P < 0.0001). Serious complication rates were similar for SG (2.4%) and RYGB (2.5%, P = 0.736). Excess body weight loss at 1 year was 13% lower for SG (60%) than for RYGB (69%, P < 0.0001). SG was closer to RYGB than lap band (LAGB) with regard to remission of obesity-related comorbidities.Q Overall complication rates among patients undergoing gastric sleeve (SG) (6.3%) were significantly lower than for gastric bypass (RYGB) (10.0%, P < 0.0001). Serious complication rates were similar for SG (2.4%) and RYGB (2.5%, P = 0.736). Excess body weight loss at 1 year was 13% lower for SG (60%) than for RYGB (69%, P < 0.0001). SG was closer to RYGB than lap band (LAGB) with regard to remission of obesity-related comorbidities.Q |
PYY levels increased similarly after either procedure. The markedly reduced ghrelin levels in addition to increased PYY levels after gastric sleeve surgery, are associated with greater appetite suppression and excess weight loss compared with gastric bypass.I (Editors’s note: both ghrelin and peptide YY effect appetite. See our obesity and genetics page for more details) PYY levels increased similarly after either procedure. The markedly reduced ghrelin levels in addition to increased PYY levels after gastric sleeve surgery, are associated with greater appetite suppression and excess weight loss compared with gastric bypass.I (Editors’s note: both ghrelin and peptide YY effect appetite. See our obesity and genetics page for more details) |
The gastric sleeve operation is able to achieve significant weight loss comparable to the gastric bypass and duodenal switch operations but with the low morbidity profile similar to that of lap band placement.J The gastric sleeve operation is able to achieve significant weight loss comparable to the gastric bypass and duodenal switch operations but with the low morbidity profile similar to that of lap band placement.J |
Duodenal Switch (DS) vs Gastric Bypass Duodenal Switch (DS) vs Gastric Bypass |
Compared with gastric bypass, duodenal switch may be associated with a greater risk of vitamin A and D deficiencies in the first year after surgery and of thiamine deficiency in the initial months after surgery.K(Editors’s note: See our Bariatric Vitamins page for more.) Compared with gastric bypass, duodenal switch may be associated with a greater risk of vitamin A and D deficiencies in the first year after surgery and of thiamine deficiency in the initial months after surgery.K(Editors’s note: See our Bariatric Vitamins page for more.) |
Although duodenal switch is associated with more bowel episodes than gastric bypass, the difference is not statistically significant. Bowel habits are similar in patients who achieve 50% estimated body weight loss with duodenal switch surgery or gastric bypass.L Although duodenal switch is associated with more bowel episodes than gastric bypass, the difference is not statistically significant. Bowel habits are similar in patients who achieve 50% estimated body weight loss with duodenal switch surgery or gastric bypass.L |
Direct comparison of Duodenal Switch toGastric Bypass demonstrates superior weight loss outcomes for DS. Importantly, the likelihood of successful weight loss (excess weight loss >50%) was significantly greater in patients following DS (12 months, 83.9% vs. 70.4%; 18 months, 90.3% vs. 75.9%; 36 months, 84.2% vs. 59.3%).M Direct comparison of Duodenal Switch toGastric Bypass demonstrates superior weight loss outcomes for DS. Importantly, the likelihood of successful weight loss (excess weight loss >50%) was significantly greater in patients following DS (12 months, 83.9% vs. 70.4%; 18 months, 90.3% vs. 75.9%; 36 months, 84.2% vs. 59.3%).M |
No patients reported dumping syndrome (after DS surgery), and marginal ulcers were not seen.N No patients reported dumping syndrome (after DS surgery), and marginal ulcers were not seen.N |
Summary of Findings When Comparing Gastric Bypass to Other Procedures Year of Study |
Lap Band Surgery vs Gastric Bypass |
Roux-en-Y gastric bypass is associated with better weight loss, resulting in a better correction of some comorbidities than gastric banding, at the price of a higher early complication rate. This difference, however, is largely compensated by the much higher long-term complication and reoperation rates seen after gastric banding.O 2012 |
Weight loss outcomes strongly favoredgastric bypass over lap band surgery. Patients treated withlap band had lower short-term morbidity than those treated with gastric bypass, but reoperation rates were higher among patients who receivedlap band surgery. Gastric bypass should remain the primary bariatric procedure used to treat obesity in the United States.A Editor’s Note: This study was published before long-term results had been published for gastric sleeve surgery. 2008 |
Collectively, data clearly point to distinct changes in dietary habits after bariatric operations which markedly differ between gastric bypass andlap band patients. Overall, it is tempting to conclude that gastric bypass operations lead to a healthier and a more balanced diet thanlap band implantations.B 2008 |
Gastric bypass seems to provide a stronger suppression of ghrelin in comparison with gastric lap band procedure. These findings are consistent with the hypothesis that suppression of ghrelin is one mechanism by which gastric bypass can reduce body weight long term, more thanlap band.C 2003 |
Mini Gastric Bypass Surgery vs Gastric Bypass |
Pending long-term evaluation, mini gastric bypass surgery seems a good alternative to gastric bypass, giving the same results with a more simple and reproducible technique.D 2008 |
Previous studies have demonstrated that hospitalization after gastric bypass increases remarkably (20% per year). The present study shows that hospitalization followingmini gastric bypass surgery instead of rising, as reported with gastric bypass, decreases by a third. Themini gastric bypass has been shown to be a short, safe successful weight loss surgery in previous work. The present study supports themini gastric bypass as a low risk procedure that decreases the need for hospitalization.E 2006 |
Both gastric bypass andmini gastric bypass surgery are effective for morbid obesity with similar results for resolution of metabolic syndrome and improvement of quality of life. Mini gastric bypass surgery is a simpler and safer procedure that has no disadvantage compared with gastric bypass at 2 years of follow-up.F 2005 |
Gastric Sleeve Surgery vs Gastric Bypass |
Compared with gastric sleeve, gastric bypass had significantly better effect in resolving type 2 diabetes mellitus, hypertension, hypercholesterolemia, gastroesophageal reflux disease, and arthritis. However, gastric bypass had higher incidence of complications and reoperation, and longer operation time than gastric sleeve.P 2014 |
Overall complication rates among patients undergoing gastric sleeve (SG) (6.3%) were significantly lower than for gastric bypass (RYGB) (10.0%, P < 0.0001). Serious complication rates were similar for SG (2.4%) and RYGB (2.5%, P = 0.736). Excess body weight loss at 1 year was 13% lower for SG (60%) than for RYGB (69%, P < 0.0001). SG was closer to RYGB than lap band (LAGB) with regard to remission of obesity-related comorbidities.Q 2013 |
PYY levels increased similarly after either procedure. The markedly reduced ghrelin levels in addition to increased PYY levels after gastric sleeve surgery, are associated with greater appetite suppression and excess weight loss compared with gastric bypass.I (Editors’s note: both ghrelin and peptide YY effect appetite. See our obesity and genetics page for more details) 2008 |
The gastric sleeve operation is able to achieve significant weight loss comparable to the gastric bypass and duodenal switch operations but with the low morbidity profile similar to that of lap band placement.J 2007 |
Duodenal Switch (DS) vs Gastric Bypass |
Compared with gastric bypass, duodenal switch may be associated with a greater risk of vitamin A and D deficiencies in the first year after surgery and of thiamine deficiency in the initial months after surgery.K(Editors’s note: See our Bariatric Vitamins page for more.) 2009 |
Although duodenal switch is associated with more bowel episodes than gastric bypass, the difference is not statistically significant. Bowel habits are similar in patients who achieve 50% estimated body weight loss with duodenal switch surgery or gastric bypass.L 2008 |
Direct comparison of Duodenal Switch toGastric Bypass demonstrates superior weight loss outcomes for DS. Importantly, the likelihood of successful weight loss (excess weight loss >50%) was significantly greater in patients following DS (12 months, 83.9% vs. 70.4%; 18 months, 90.3% vs. 75.9%; 36 months, 84.2% vs. 59.3%).M 2006 |
No patients reported dumping syndrome (after DS surgery), and marginal ulcers were not seen.N 2006 |
For further comparison of gastric bypass surgery to other procedures, see our Types of Bariatric Surgery page.
Quiz: Which Weight Loss Surgery Is Best for You?
Start to Finish
7 Steps to Long-Term Weight Loss
Start to Finish – 7 Steps to Long-Term Weight Loss
Step 1: Start Working with a Weight Loss Surgeon As Soon as Possible
Surgeons will help you effectively navigate the various procedure choices, pre-surgery steps, financing, and insurance options:
- As a first step, many surgeons offer a free initial consultation or a free local seminar or webinar to give you a better understanding of what to expect.
- Many will also provide a free insurance check to help you figure out how much insurance will cover, and, if necessary, appeal any denials or find additional financing. Most insurance companies require you to complete a medically supervised diet and exercise program before they will approve your surgery, so your surgeon will set this up for you if you haven’t done so already.
- Your surgeon will also push you towards new habits that will be essential to long-term success after surgery. Many surgeons will recommend that you attend support group meetings so you can listen to feedback from actual patients.
Step 2: Two Weeks Out: Prepare for Surgery
By 2 weeks out you will have completed your pre-op tests, physical, and any other necessary steps required by your surgeon or insurance company. You should have insurance approval (if applicable), and you should be well on your way towards developing your new long-term lifestyle and diet habits. In the week or two leading up to surgery you’ll be seeing the hospital pre-surgery department for an EKG, blood work, and any last minute instructions or other pre-op tests. You’ll see the surgeon one more time for consents, a pre-operative physical, and any last minute details. The night before surgery you’ll be asked to not eat or drink anything starting at midnight.
You’ll be asked to arrive at the hospital at least two hours prior to surgery to allow for prep time. The gastric bypass procedure itself will take about 4 hours to perform. For the first few hours after surgery, you probably won’t be awake to remember it, but you’ll have one-on-one attention from someone on your surgical team to manage your pain and monitor your vitals. Click here for more about what to expect in the hospital.
Most gastric bypass patients are in the hospital for 2 or 3 days total. You will probably not be allowed to eat or drink anything for at least 24 hours after surgery, and your surgeon will want you to get up and walk around as soon as possible to start the healing process. You’ll be discharged as soon as your surgeon is confident that you are well on the road to full recovery. You’ll likely need someone to drive you home from the hospital and care for you for at least a few days following surgery. Full recovery generally happens within 4 to 6 weeks. Click here for more about the recovery process.
Step 5: Adjust to Your New Post-Surgery Diet & Lifestyle
Over the course of the first 6 weeks following surgery you will slowly transition from a sugar-free clear liquid diet to your “new normal” gastric bypass diet. You should also continue your transition into a more active lifestyle. You will feel full sooner, you may feel less hungry generally, and you should start to experience significant weight loss within a couple weeks. Your surgeon’s dietitian or nutritionist will help you determine an appropriate diet. See the Diet & Life After section of this page for more information.
Step 6: Attend Support Groups Regularly
Regular weight loss surgery support group participation has been found to lead to the following benefits:
- Reduce post-op recovery time
- Lead to as much as 12% more long-term weight loss
Your surgeon will be able to recommend an in-person group near you.
For the first year, your surgeon will most likely schedule follow up visits. Shortly after surgery, they will be weekly then transition to every four weeks, and, later, once every few months to ensure that you are recovering well and to answer any questions you may have. Subsequent doctor visits will be scheduled on an as-needed basis along with annual check-ups.
Help & Support
Patient Experiences & Ask the Expert
Help & Support*
Patient Experience & Ask the Expert*
We would love to hear your experiences with the gastric bypass surgery. Much like how support groups help others, your insights are invaluable to making sure other people have the tools to meet their goals.
We would also be happy to answer any questions you may have about gastric bypass surgery.
Please use the form below to share your experience or ask a question…
Questions From Other Visitors*
Click below to see contributions from other visitors to this page.
Find a Gastric Bypass Surgeon
DISCLAIMER : Information received via BariGroups group meetings or during coaching sessions should NOT be relied upon for personal, legal or medical decisions and you should consult with your doctor or other licensed professional before beginning and during any course of medical treatment. By using BariGroups, you are confirming that you agree with our Terms & Conditions (click here to review).
I agree